Breaking down the microbiology world one bite at a time
Resilience is key
Antimicrobial resistance is a growing concern in the scientific community. In fact, a recent study estimated that about 4.95 million deaths in 2019 were associated with bacterial antimicrobial resistance. Although antimicrobial resistance is studied by multiple groups across multiple pathogens, bacteria seem to be gaining resistance at faster rates than ever before. This has led many scientists to seek out how bacteria gain and maintain their resistance, including the authors of this paper.
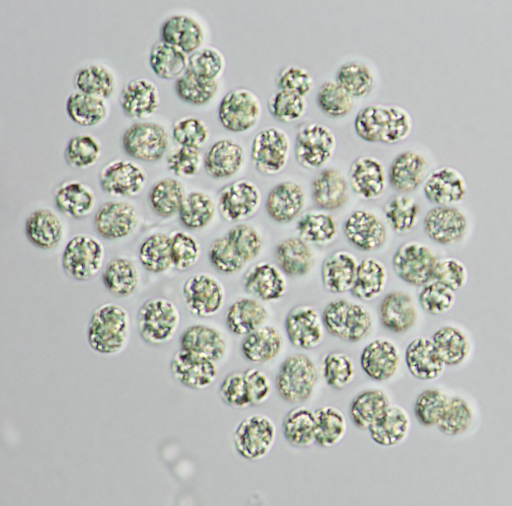
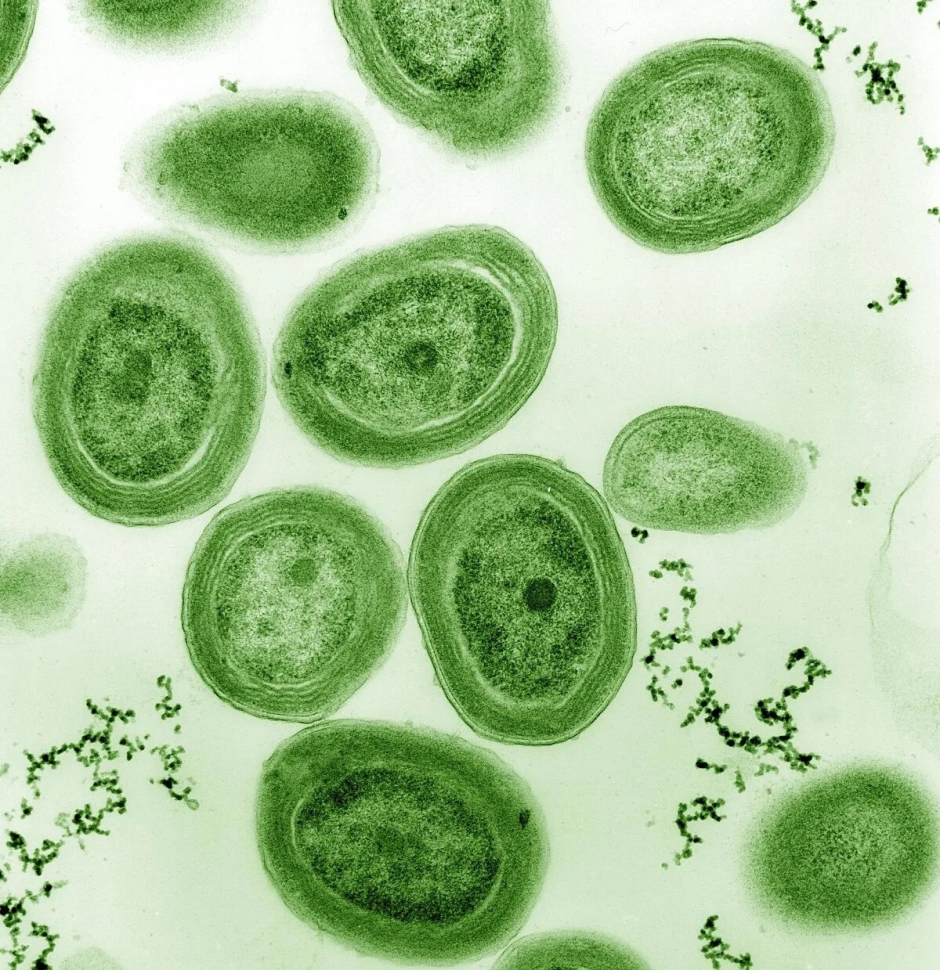
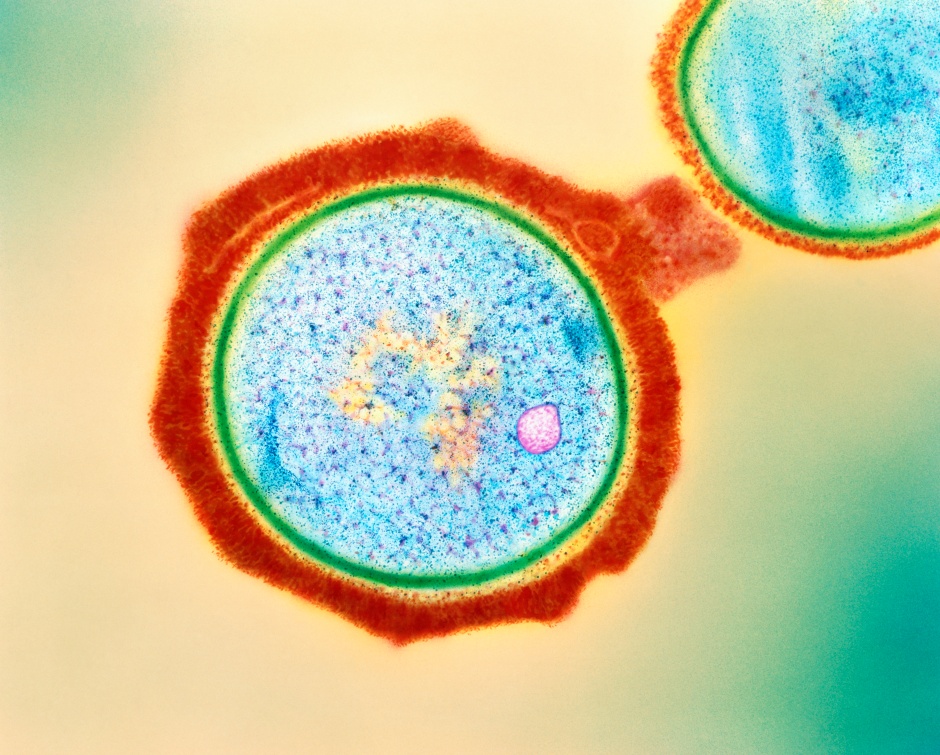
In this study, the authors predicted that mutations in genes that persisted in antibiotic-resistant strains of bacteria would provide insight into what molecular mechanisms are important for resistance. To do this, they analyzed clinical isolates of Mycobacterium tuberculosis (Mtb), which is the bacteria that causes tuberculosis (TB). Mtb is historically a persistent organism, and has even gained resistance to multiple antimicrobials, making it a great candidate for studying antibiotic resistance mechanisms.
Identifying a key player in antimicrobial resistance
To study how Mtb evolves antibiotic resistance strategies, the authors looked at the genomes from over 50,000 clinical isolates of tuberculosis. Using statistical analysis, they noticed that one gene was mutated in most of their strains, resR. resR is a regulatory gene, meaning that it controls the activation and deactivation of many other genes. This finding was promising, as it likely meant that resR was a key player in the antibiotic resistance mechanism of these strains.
However, this wasn’t exactly the case.
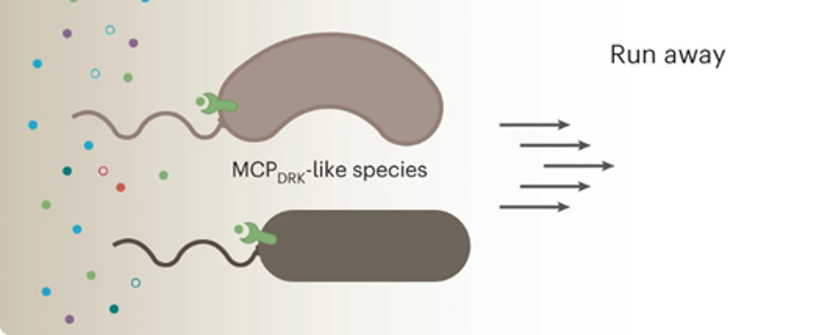
Antibiotics commonly used to treat TB killed strains with resR mutations at the same rate as strains without these mutations. So, resR isn’t responsible for antibiotic resistance in a classical sense. However, the authors noted an interesting phenomenon in strains that had the resR mutation. When these strains were given high concentrations of antibiotics, then were grown without any antibiotics, resR mutants recovered much faster (up to 50%!) than strains without a resR mutation. The authors termed this phenomenon antibiotic resilience.
How do bacteria gain antibiotic resilience?
The concept of antibiotic resilience (also called a post-antibiotic effect) isn’t actually all that new of an idea. In fact, this phenomenon has been recognized by the scientific community for decades and has been observed across a variety of bacteria. However, the mechanism of antibiotic resilience isn’t well understood. So, the authors of this paper started to focus on what genes are regulated by resR to see if those genes were contributing to antibiotic resilience.
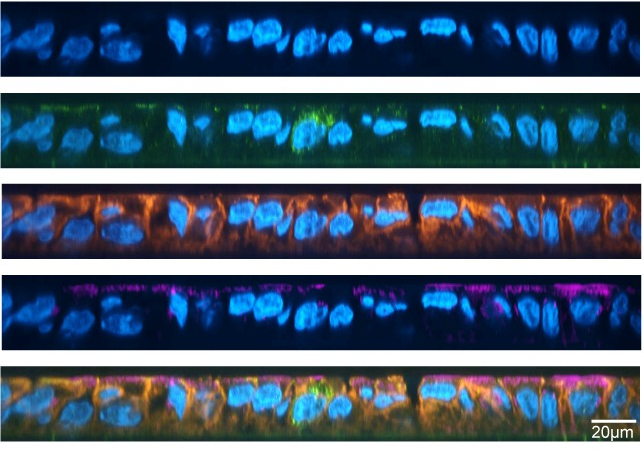
To do this, the authors used a combination of genome sequencing and a DNA-to-protein binding assay to identify sequences of DNA that ResR (the protein encoded by our key gene of interest, resR) can bind to, as direct binding to DNA usually indicates that a protein is regulating it. Interestingly, they found one region that not only was a site for ResR binding but was also associated with Mtb antibiotic resistance. This site was the whiB2-fbiA intergenic region. Since intergenic regions are often sites of regulation of genes, the authors used RNA sequencing to determine which genes had altered transcription in resR mutant strains. Supporting their previous finding, the resR mutants had about two times more whiB2 transcript levels compared to strains without resR mutants.
So, what does whiB2 even do? The WhiB2 protein is a regulator of cell growth in mycobacteria, which is a group of bacteria that includes Mtb. Indeed, the antibiotic-resilient strains with resR mutants that were previously identified (and strains with mutants in the whiB2-fbiA intergenic region itself) not only altered the activation rate of whiB2 gene expression, but they also affected the cell size! These observations clearly linked whiB2 to antibiotic resilience. Although whiB2 seemed to be the key gene involved in antibiotic resilience, it had a partner that could potentially play a role in this mechanism.
Another player enters the game.
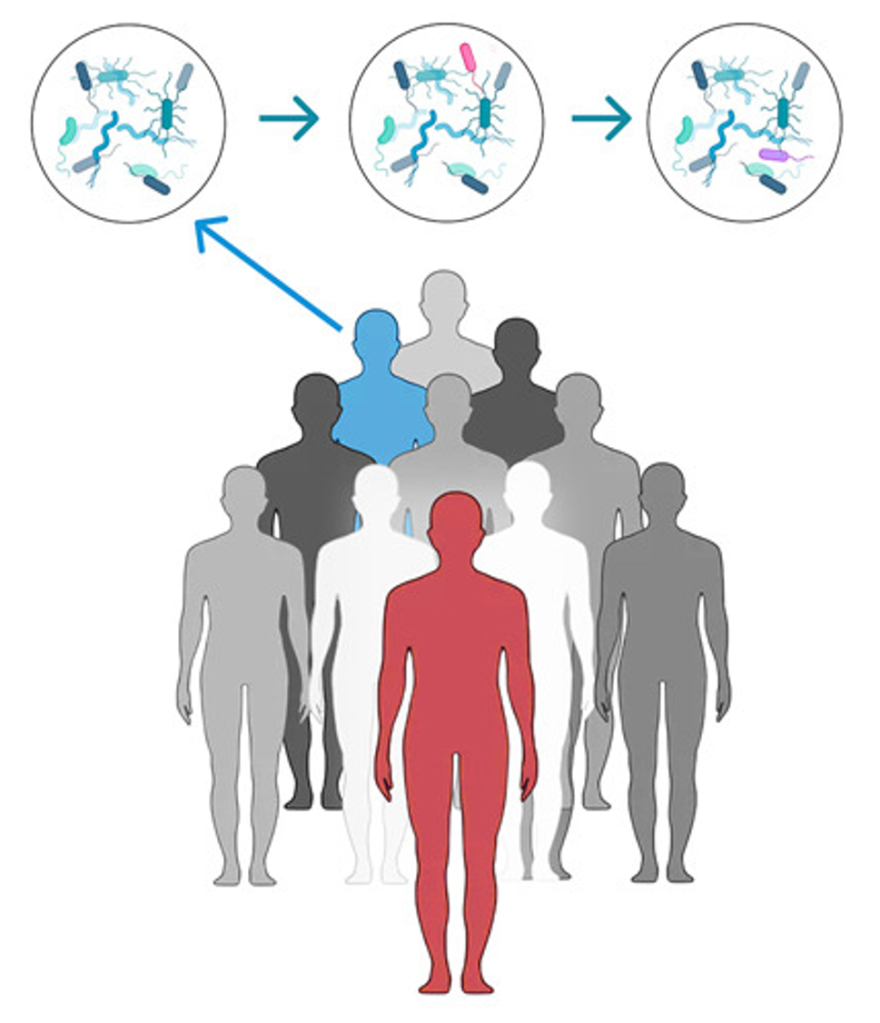
The WhiB2 protein wasn’t unfamiliar to the authors of this paper. In fact, a lot is known about this regulator in another common pathogen, Streptomyces (well-known for causing strep throat). In Streptomyces, WhiB2 acts with its counterpart, WhiA to regulate when the cell starts to divide. Based on this, the authors thought that whiA might be highly mutated in antibiotic-resilient strains, similarly to resR. When they looked at their original sequencing data, they found that about 7% of their clinical isolates had mutations in whiA, resR, and in the whiB-fbiA intergenic region. They also noticed that strains of Mtb with these mutations were highly associated with canonical antibiotic resistance, even in strains that were isolated in different countries.
The most interesting data however involved recurrent TB. Many patients that provided samples for this study had more than one episode of TB, suggesting that the strain of Mtb causing their illness was resisting treatment. Of the 36 patients that failed treatment for recurring TB in their clinical study, 22.2% had mutations in the key players involved in antibiotic resilience (whiA, whiB-fbiA, or resR). Even more striking, five patients had an increase in mutations in the key players during their second TB episode compared to their first TB episode.
So what does this all mean?
Antibiotic resistance continues to be a huge problem in microbiology, and studies that uncover potential mechanisms of how this happens are key to solving this issue. Using clinical isolates instead of strains of Mtb that are only grown in the laboratory is a great way to understand the characteristics of bacteria that are actually circulating in hospitals. Furthermore, now that we know that Mtb can gain antibiotic resilience, we can look out for this phenomenon when we culture isolates from the hospital. This will give physicians insight on when the antibiotic they’re prescribing isn’t tough enough to get rid of the resilient bacteria.
Link to the original post: QINGYUN LIU et al., Tuberculosis treatment failure associated with evolution of antibiotic resilience. Science 378;6624
Featured image: Ernesto del Aguila III, NHGRI.