Breaking down the microbiology world one bite at a time
Gut prepares for war against invaders using the complement system
Invaders are bad for the body. Therefore, the body has multiple ways of detecting invaders and attempting to kill them. The complement system is one such method for the body to mark invaders for the immune cells in the blood and other bodily fluids. A special protein marker called complement component 3 (C3) is deposited on the surface of bacterial cells, tagging the invaders, making it easy for the immune cells (the army of the body) to attack them.
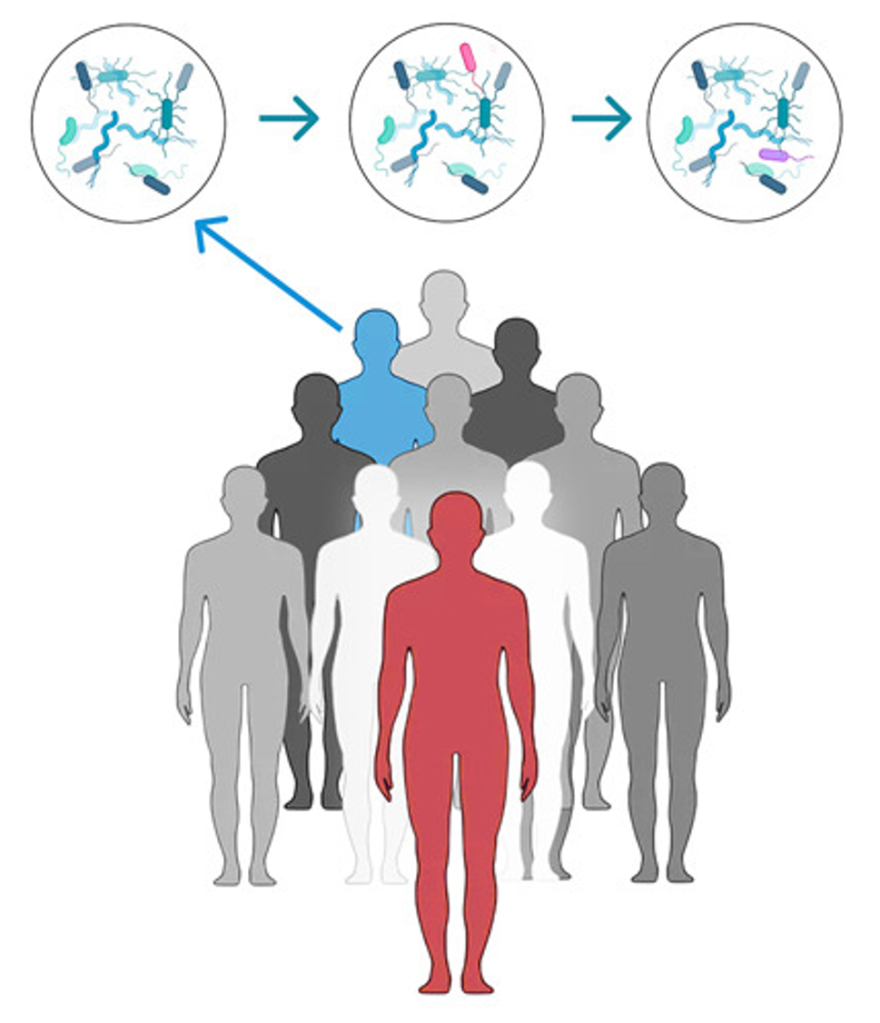
This new study shows that C3 is produced in the intestine by microbiota. The authors showed that antibiotic mediated depletion of microbiota led to a reduction of C3 levels in the intestine. The authors tested human feces from healthy donors and observed varying levels of C3 protein. To understand the complicated relationship between the C3 levels and the gut microbiota, they transplanted feces from the human donors with high and low levels of C3 into germ-free mice and the mice with the human microbiota copied the C3 levels seen in the humans i.e., the mice with high C3 human microbiota also had high C3 levels and the mice with the low C3 human microbiota had low C3 levels.
The authors also tested mice from different commercial companies and identified mice from two different mice supplier companies where mice from one company had low C3 levels while mice from another supplier had high C3 levels. The mice from the two suppliers had different microbiota and therefore had varying levels of C3. When these mice were co-housed, they exchanged their microbes which led to all mice having the higher level of C3 seen originally only mice from the second company.
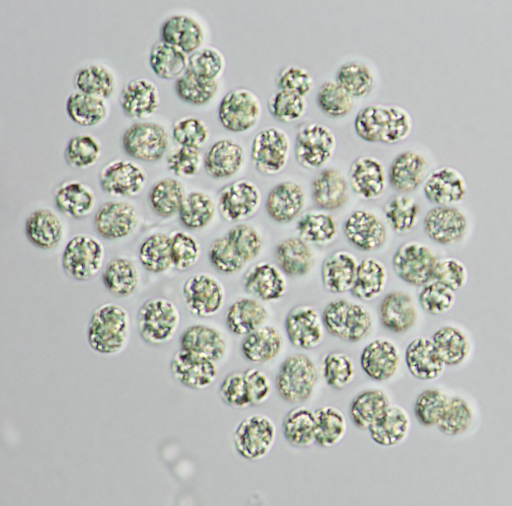
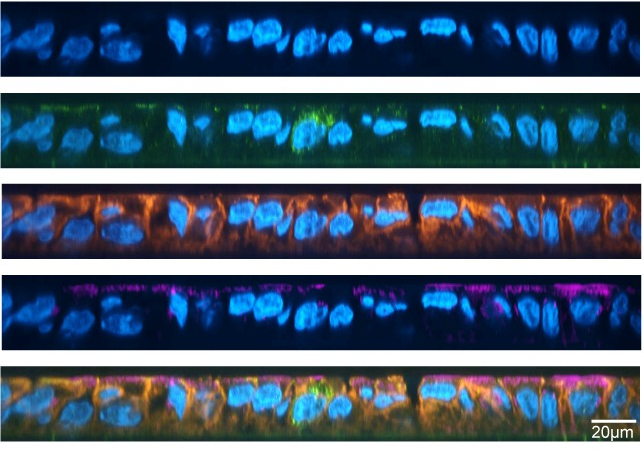
The authors sequenced the microbiota present in humans and mice and compared individuals with high C3 to individuals with low C3 levels to determine that the presence of Prevotella correlated with C3 levels. Mice that have only Prevotella living within it have increased C3 levels. This suggests that complex microbial interactions are likely to mediate the induction of C3. To understand which host cells in the body can produce C3, the authors looked at the genetic information encoded in the host cells. DNA in the host cells is converted to RNA transcripts by specialized machinery, which further transforms to proteins required for the smooth functioning of cells. RNA sequencing is a method to reveal the sequence of the RNA transcripts of a cell. In this study, the authors performed single-cell RNA sequencing. It is a method to look at the transcripts produced at a single cell level rather than the tissue level. By not limiting their findings to tissue level, the researchers increase the resolution of their findings, thus revealing the diversity of individual cells in a tissue. In this study, through single-cell sequencing, the authors found that a subtype of cells present in the connective tissue known as stromal cells were the major producers of C3 under homeostasis (non-inflamed situation).
Do these C3 proteins coat the usual residents, known as commensals that are commonly present in the intestine? Comparison with mice deficient in C3 protein revealed that these C3 proteins did not damage the good microbiota. Prevotella and other microbes in the colon stimulate stromal cells in the aggregates of immune cells called isolated lymphoid follicles to produce C3 protein. Investigations showed that certain markers present on the outer membrane of some bacteria can bind to receptors on the stromal cells to stimulate C3 production, revealing why some microbes correspond to high C3 levels while others do not.

In an attempt to understand the physiological relevance of this system, the authors studied how varying levels of C3 in the gut can affect protection against enteric pathogens using Citrobacter rodentium as a model pathogen. Higher C3 protein levels in the lumen offered increased protection against the pathogen with C3 coating the Citrobacter rodentium, enabling immune cells to attack it and handle the infection better. The authors also saw that upon intestinal pathogen infection, C3 levels inside the gut increased. The C3 protein marks out all the bugs present in the body allowing for certain specialized immune cells to eat them up, thus preventing the bugs from destroying the body.
The presence of C3 protein in inflamed and non-inflamed states yet only causing havoc during infection is an excellent demonstration of how fine-tuned our immune system is. This has profound clinical implications for patients suffering from gut disorders like irritable bowel disease. They have these marker protein deposits in the body which can explain why immune cells incorrectly attack healthy human tissue. The study is interesting because it suggests that perhaps modulating the microbiota might enable patients to lower their complement levels in the gut. This idea warrants further study. Now you know how the microbiota present in the body can control the marker levels and therefore the immune system’s functioning.
Link to the original post: Wu M, Zheng W, Song X, et al. Gut complement induced by the microbiota combats pathogens and spares commensals. Cell. 2024;187(4):897-913.e18. doi:10.1016/j.cell.2023.12.036
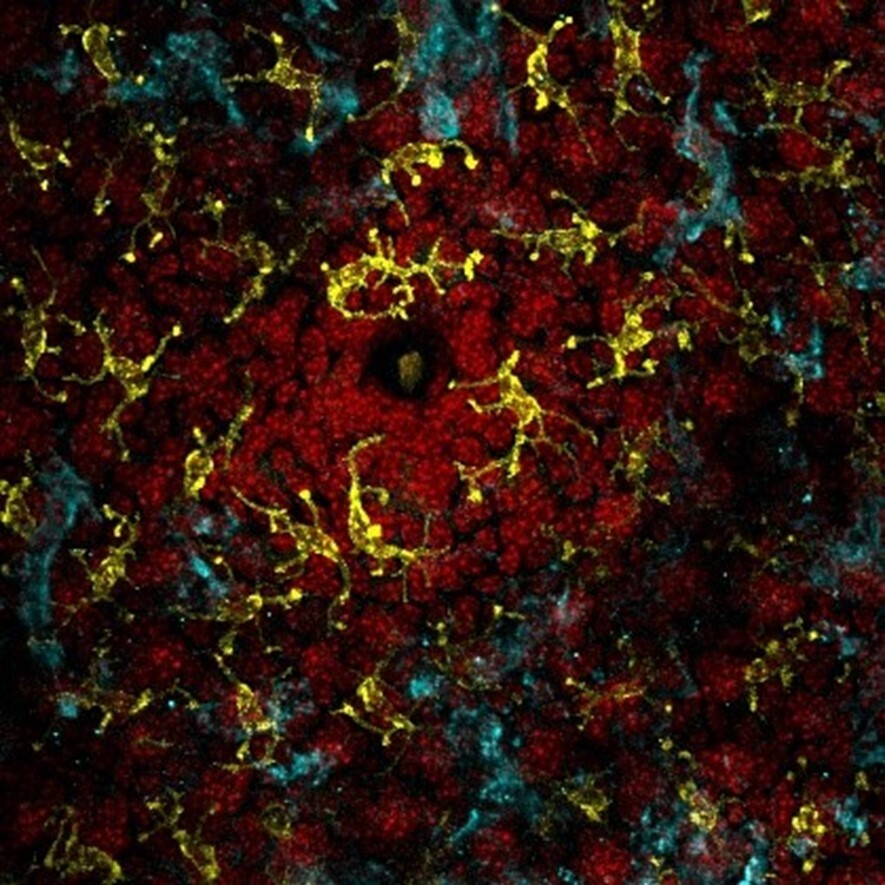
Featured image: “Enteropathogenic E. coli on human intestinal cells” is licensed under CC BY 4.0.