Breaking down the microbiology world one bite at a time
Diabetogenic viruses: Leveraging of the virus – to fight the virus
For quite some time, diabetes mellitus (DM) – a metabolic disease causing high blood sugar – has been a part of society. Written titbits on observations relating to diabetes have been documented as early as 1500 BC [more on the history of diabetes mellitus].
Today half a billion people suffer from diabetes. Diabetes is a complex multifactorial disease; with causes being either genetic or lifestyle-based and over time can lead to multi-organ failure. Diabetes doesn’t follow a straight course of infection and oftentimes can be aggravated by an individual’s circumstances. From family history and environmental cues to pre-existing medical conditions, anything could be a trigger for diabetes. In fact, a universal cure for DM is not attainable because a definitive or unique cause for diabetes is yet to be established.
Researchers have since shifted their focus to regulating/preventing the various trigger factors for diabetes. Quite unsurprisingly viruses have long been associated with DM. Called diabetogenic (producing- or causing diabetes) viruses, they have been reported to initiate as well as accelerate diabetes. Few vaccines have been hypothesized against them but none are approved yet.
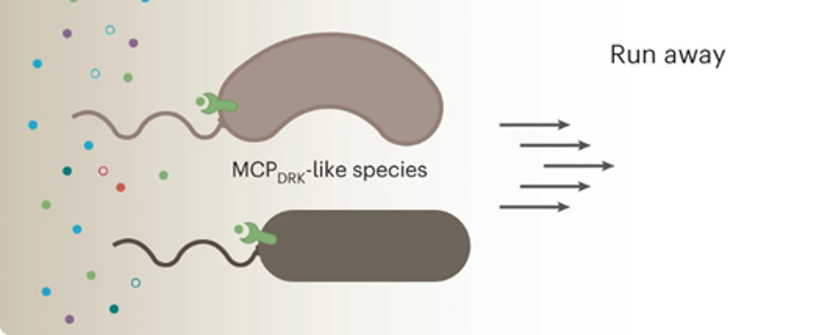
Regularly monitoring blood sugar levels and being on the lookout for further complications are the two primary tools for diabetes management. Undetected diabetogenic viral infections can be a severe threat to these management techniques. This is because the viral load being too low, isn’t suitable for molecular detection but efficient enough to contribute to the aggravation of DM. This could lead to rising blood sugar levels without any detectable cause which can subsequently affect the treatment process as well as the overall health of an individual. But how does this diabetogenic virus work exactly?

Diabetes, pancreas, and diabetogenic viruses
Diabetes mellitus is divided into two categories – type 1 and type 2, depending on insulin action. Insulin is a chemical messenger for our cells. Our body produces insulin specifically in the organ called the pancreas. Insulin signals the cells to take up glucose formed by the breakdown of the food we consume and use that to make energy. In type 1 DM, due to a genetic predisposition, there is defective insulin production by the body, while in type 2 DM an individual’s cells acquire insulin resistance. In someone with diabetes, when they either don’t have enough insulin or their body doesn’t respond well to it, the ability to use glucose by their cells stops and therefore leads to glucose buildup in the blood.
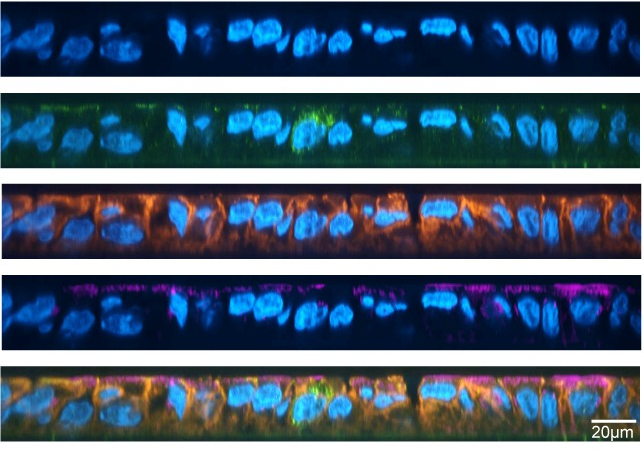
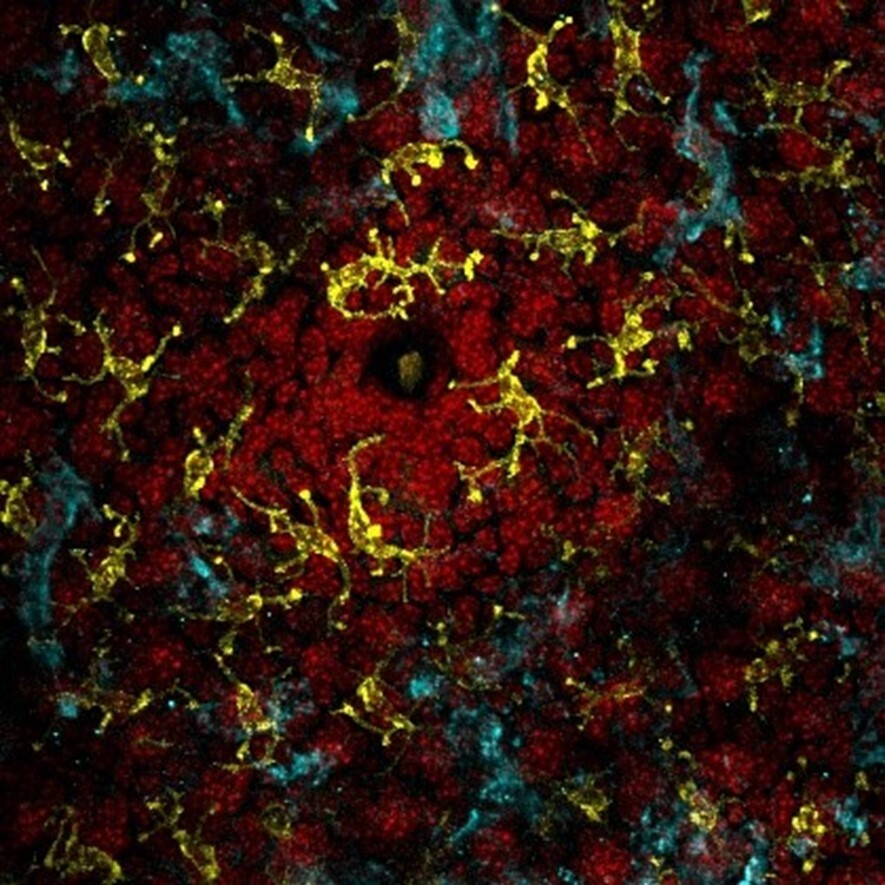
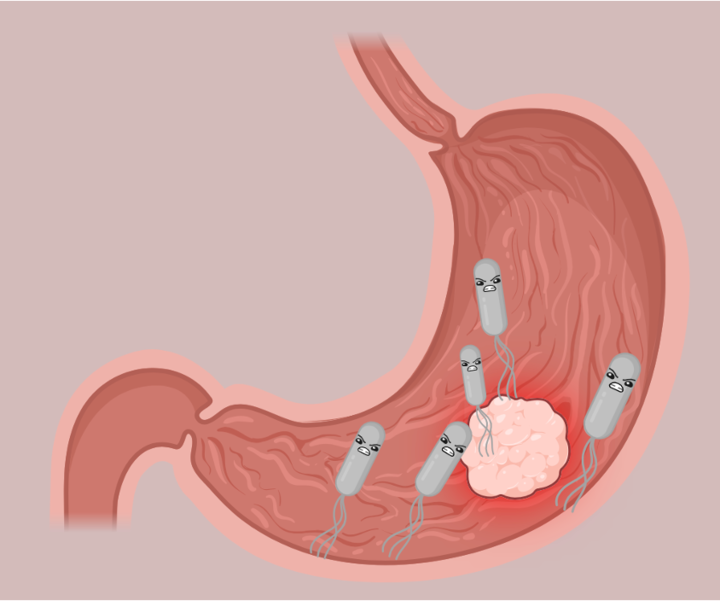
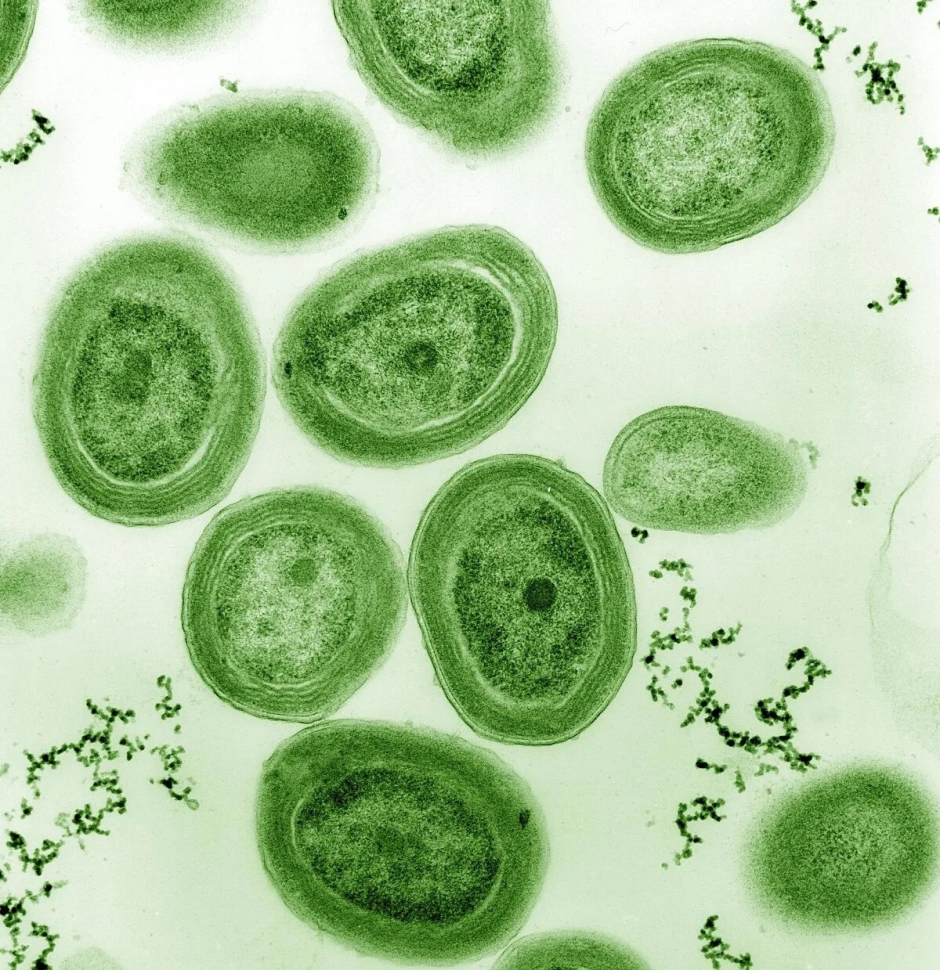
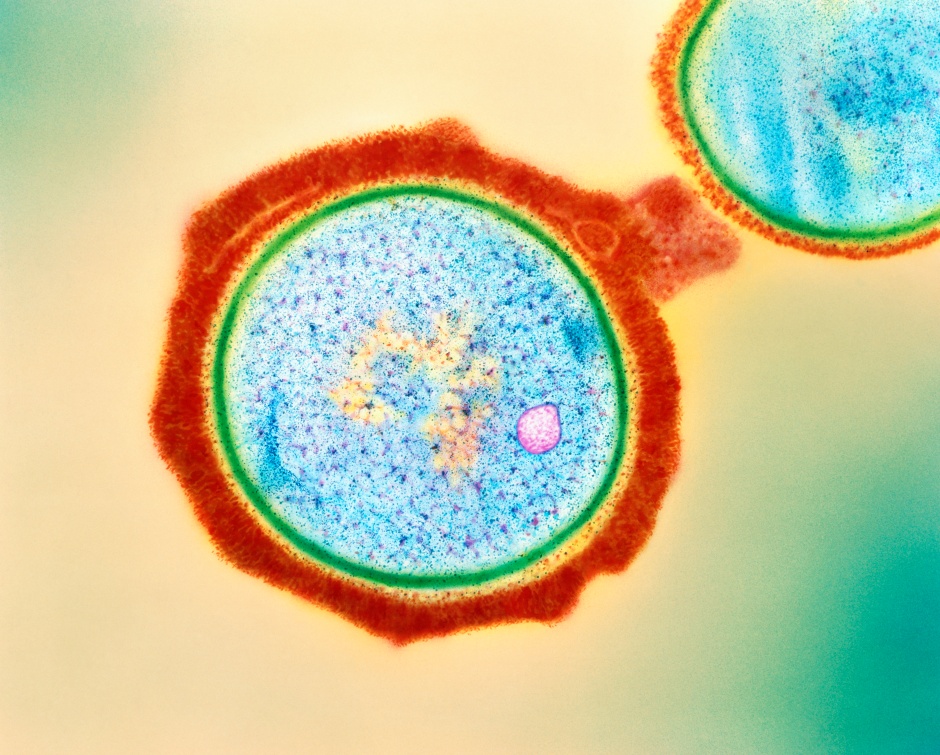
Diabetogenic viruses, being the sneaky little beings, target the pancreas. They destroy the cells that produce insulin in the pancreas and disrupt the body’s metabolic system. Several viruses, some with stronger associations while others weaker have been reported to be diabetogenic. But the most firmly documented diabetogenic viruses have been from the Enterovirus family. Some of the other common diseases caused by this family include Polio, Bornholm disease, hemorrhagic conjunctivitis, and hand-foot-and-mouth disease.
Of the Enterovirus family, Coxsackievirus B4 (CVB4) is considered to be the most diabetogenic. CVB4 RNA genomes have been isolated from lab studies on human pancreatic cells as well as post-mortem pancreatic reports of children suffering from type 1 DM. CVB4 infection starts or speeds up diabetes progression by assisting the human immune system to attack its own pancreatic cells, resulting in insulin deficiency. This, in turn, causes high blood sugar levels with dire consequences.
While a vaccine seems the most probable therapeutic choice against them, designing an Enterovirus vaccine is quite a challenge. This is because Enterovirus includes several serotypes but an insufficient understanding of the serotype-disease relationships. Serotypes, basically, refer to microbes belonging to the same species (bacteria, virus, etc.) but with some minute differences. It acts like a name tag for the bacteria or virus. It’s kind of like how we can tell people apart by their names, even if they look similar. Serotypes help scientists identify and categorize them based on their certain characteristics. The enteroviral serotypes undergo continuous re-evolution, which makes it difficult for the researchers to pinpoint particular serotype-disease relationships. But researchers might have finally found a way around it!
Leveraging of the virus – to fight the virus
In a recent study, researchers tried to better understand how these diabetogenic viruses can be effectively neutralized in infected human cells. Previous studies attempted to target diabetogenic viruses using traditional strategies, but none were successful. This study attempted a more modern approach against diabetogenic viruses by employing a virus-like particle (VLP) for vaccine design.

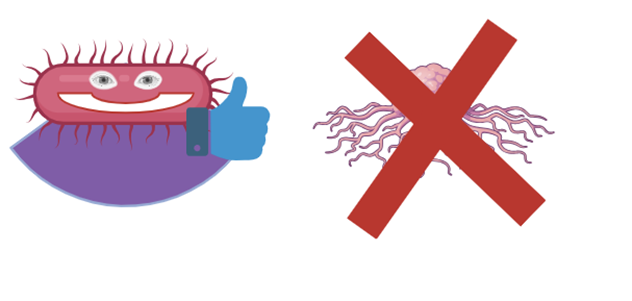
VLPs resemble viral particles but lack DNA and RNA, making them incapable of infecting humans. But they are highly immunogenic or capable of eliciting an immunological response from the body. Several virus-like particles (VLPs) generated from viruses are now being employed as vaccinations. The methodologies utilized in this work were comparable to those used in earlier VLP-based vaccination studies. They constructed a CVB4 vaccine using the major Coxsackievirus B4 antigen viral protein-1, VP1. Coxsackievirus B4 VP1 is important as the virus interacts with human cells through it.
After collecting the VP1-containing viral cells, the researchers here purified and chemically characterized them to check if they resemble the CVB4 viral particles. The efficiency of the VP1-VLP vaccine in protecting from CVB4 infection was then studied by injecting the vaccine into mice models. The mice group with the VP1-VLP vaccine were able to resist infection by both the diabetogenic (CVB4E2) and non-diabetogenic strains (CVB4JBV) of Coxsackievirus B. Furthermore, many VLP vaccines require adjuvants (-chemicals added to the vaccine that help increase its effectiveness). However, the present vaccine was able to achieve high effectiveness against the virus through a very simple purification process, without any adjuvants.
The group predicts that the use of sophisticated vaccine purification techniques could probably increase vaccine efficiency more in the future. They also monitored if the mice used in the study had any visible changes like body weight, but all mice subjects were noted to be perfectly healthy. Conclusively, the vaccine was effective 90-100% against the two strains of Coxsackievirus B infections.
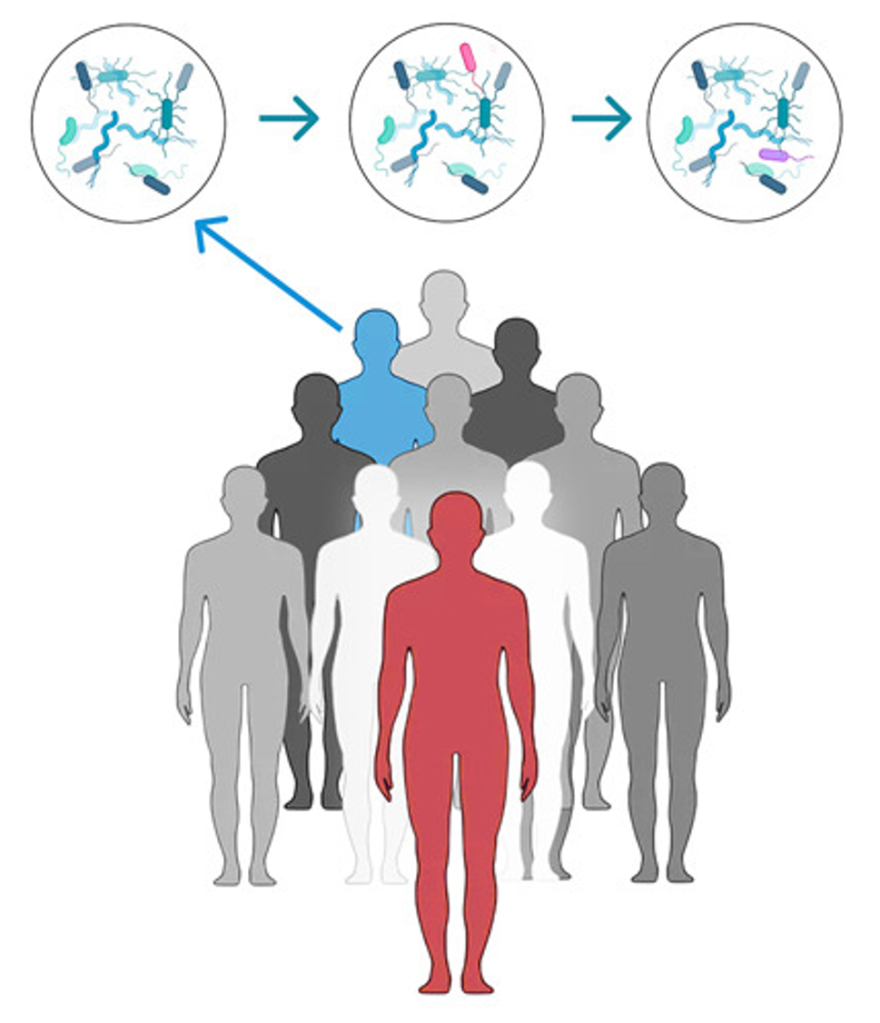
Screening and developing effective vaccines is an expensive process. This study is an important step in the fight against diabetogenic viruses and DM1 for a couple of reasons. For instance, future implementation of this study in larger study cohorts offers the possibility of both developing VP1-VLP as a marketable vaccine and paving the way for furthering VLP-based vaccine studies against other diabetogenic viruses. With a steadily increasing trend in global diabetes cases every year, studies such as the one discussed here have become of utmost importance.
Link to the original post: Gharbi, Jawhar, et al. “Viral Protein VP1 Virus-like Particles (VLP) of CVB4 Induces Protective Immunity against Lethal Challenges with Diabetogenic E2 and Wild Type JBV Strains in Mice Model.” Viruses vol. 15,4 878. 29 Mar. 2023, https://doi.org/10.3390/v15040878
Featured image: Freepik