Breaking down the microbiology world one bite at a time
Vax the Bats! Can bat herpes help stop the spread of rabies?
Thanks to global vaccination campaigns, it has been possible to tame some of the world’s most vicious viruses. The key to reducing outbreaks is to stop viruses from spreading easily. Public health measures like social distancing, increased sanitation, and wearing masks are good ways to reduce transmission, but vaccination remains the most effective as it blocks the route of transmission. Without the ability to spread, viruses cannot multiply, and the number of infectious viral particles decreases. This strategy led to the eradication of smallpox, and today it is used to reduce the burden of many different viral diseases. But even the greatest defenses have weaknesses. Wild animals that harbor viruses can be difficult to vaccinate and have the potential to spread the disease to humans. In a recent study, researchers explored a new type of vaccine that could potentially eliminate viruses in wild populations.
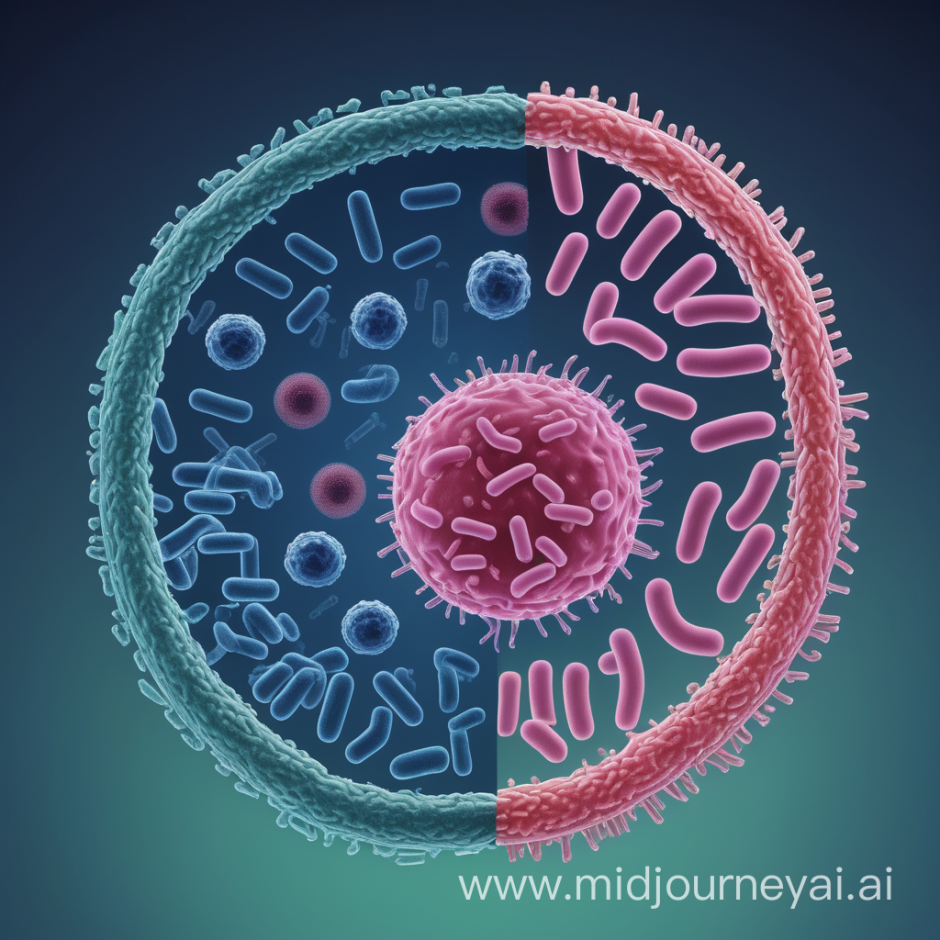
Rabies is a notorious disease caused by viruses in the Lyssavirus genus. These viruses infect the nervous system and cause unusual symptoms such as confusion, muscle spasms, and even a fear of water. Animals infected with rabies become sickly and aggressive, causing them to bite other animals and sometimes humans, spreading the disease. Once symptoms appear, rabies is almost always fatal. Preventing transmission of the virus is crucial but not easy. Unlike other viruses, rabies has a wide host range and can infect most warm-blooded mammals. Some of these animals are difficult to vaccinate, making them susceptible to infection. If left unrestricted, a virus can spread and multiply within an animal population, creating a reservoir of the virus that has the potential to spillover into humans at any moment. Without a way to manage viral reservoirs, outbreaks of rabies in humans will continue to be a problem.
In Latin America, vampire bats are a reservoir for rabies virus and have been the cause of recent outbreaks in humans. As their name implies, vampire bats’ main food source is blood. Vampire bats have razor-sharp teeth and compounds in their saliva that inhibit the blood-clotting of their prey. These features also make it easy for vampire bats to transmit rabies to other bats and animals. Due to human destruction of their natural habitats, vampire bat activity is increasing in agricultural areas, and livestock have become their preferred food source. A field of cows can quickly become a bat buffet and breeding ground for spillover events.
The current way to control vampire bat-transmitted rabies is by culling bat populations using poison which is both inhumane and ineffective. Culling causes bats to flee to new locations, which spreads the virus even more.
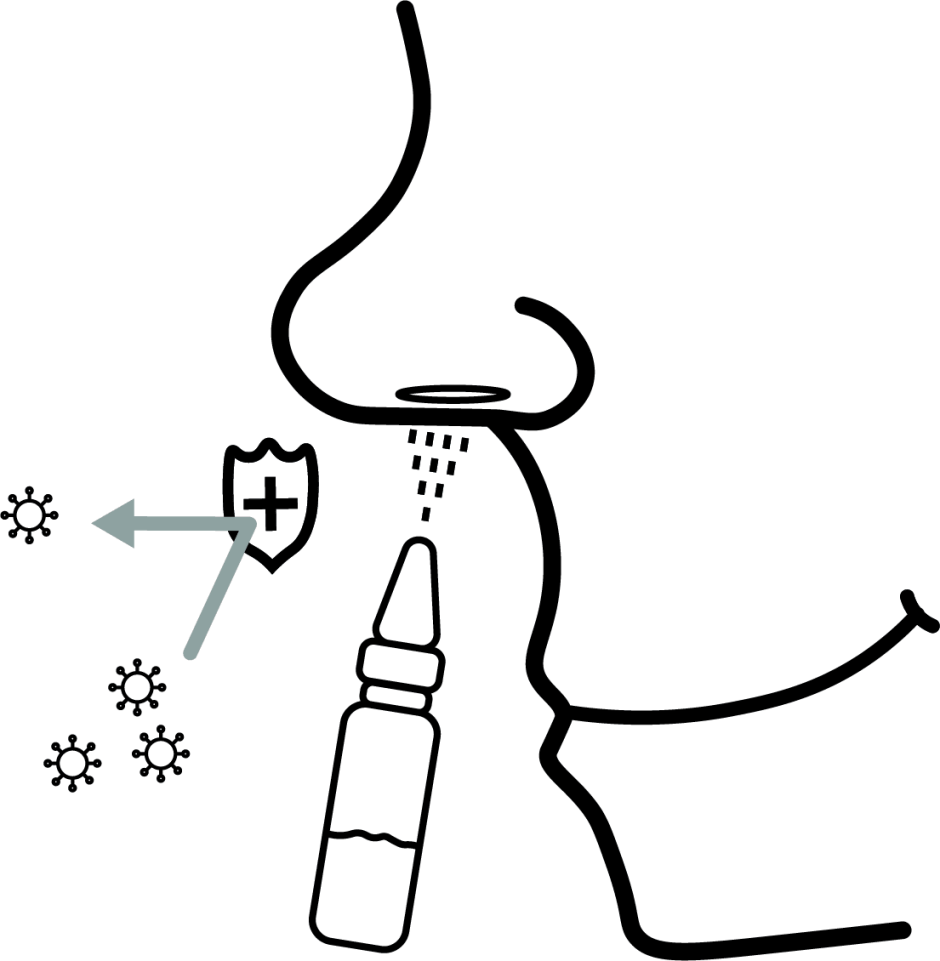
Attempts to develop a practical vaccine for bats have been unsuccessful. Domesticated animals are relatively easy to vaccinate through injections. If you have a dog or a cat, you probably take them to the veterinarian for a rabies shot every few years. Routine vaccination ensures that your furry friend stays protected from rabies while reducing your risk of contracting the virus. Pet vaccination efforts have been so successful that canine-transmitted rabies is close to being eradicated in the Americas. Vaccinating wild animals is a little more challenging, but it is possible. For carnivores (i.e. raccoons, skunks, and foxes), bait is spread in their known habitats to deliver vaccines orally. However, neither vaccination strategy works for bats. Bats roost in remote locations that are difficult to access, making it hard to capture a lot of them to deliver a vaccine. Since vampire bats only drink fresh blood, using bait to give an oral vaccine is not an option. Luckily, transmissible vaccines offer a solution.

Biology might have given rabies virus a way to get around current vaccination strategies, but it also has provided a potential solution. With some modifications, viruses have been used to make vaccines for a while. Live vaccines are made by weakening a pathogenic virus to a point where it no longer causes severe disease symptoms but still produces an immune response. In their weakened state, the virus in a live vaccine cannot multiply and spread to others. Some viruses are naturally nonpathogenic and can infect their host with mild or no symptoms. Transmissible vaccines are a developing technology that uses these viruses to our advantage.
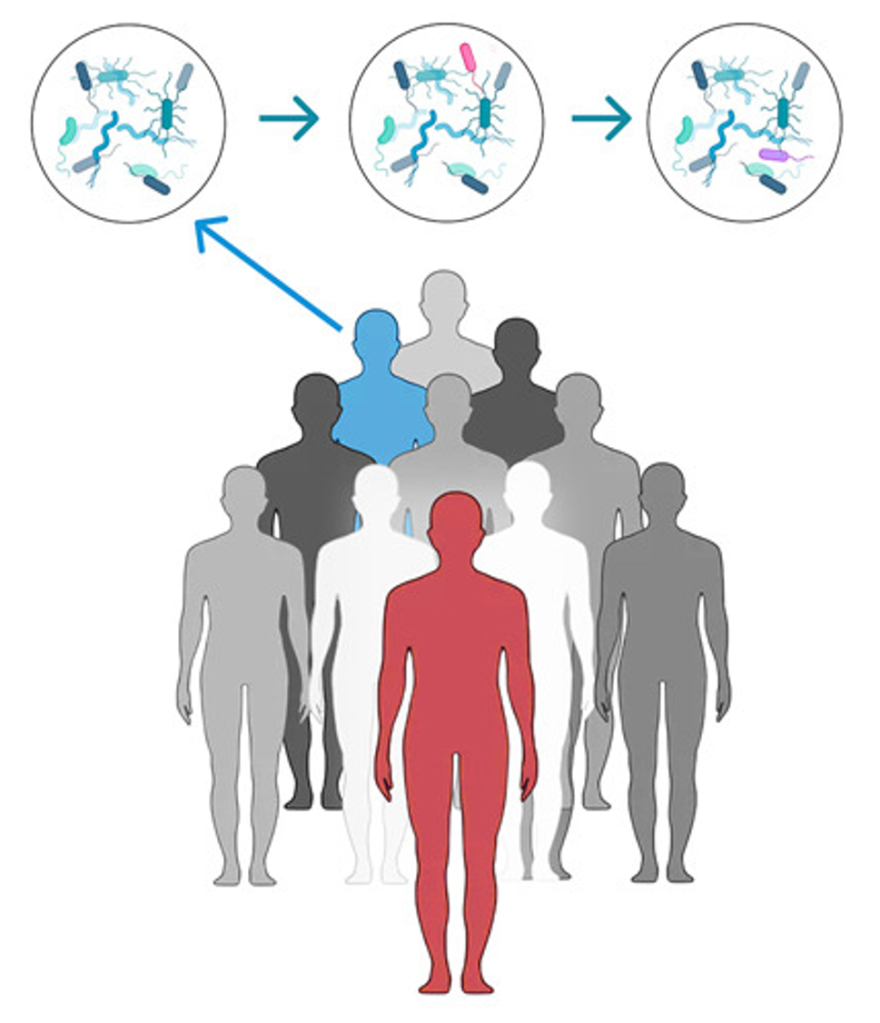
These viruses would be used to create a transmissible vaccine by bioengineering the nonpathogenic virus to express a protein of another virus. This will trigger an immune response to the pathogenic virus without causing disease symptoms. More importantly, a transmissible vaccine could be passed between individuals, making it easier and less costly to reach herd immunity in a population. Despite the potential benefits, transmissible vaccines are far from being used; more research is needed to ensure they are implemented safely and efficiently. Recent findings from a research team in Glasgow have brought the world one step closer to using transmissible vaccines to combat the rabies virus.
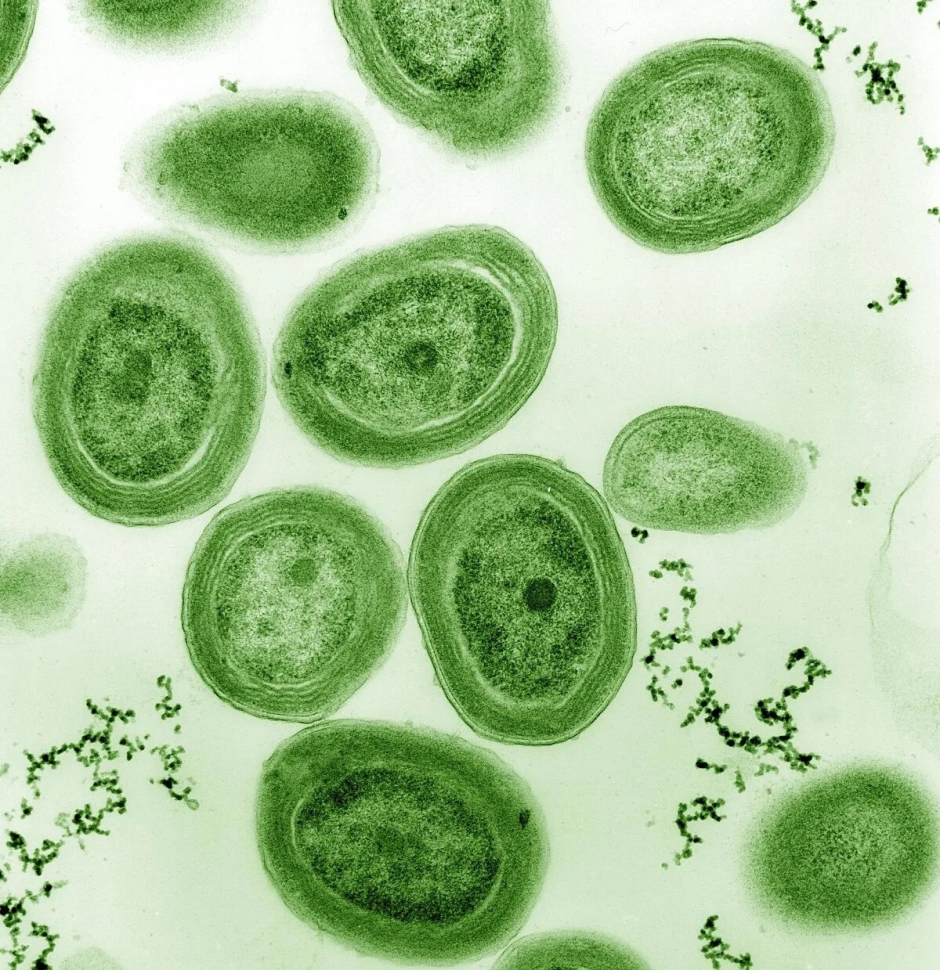
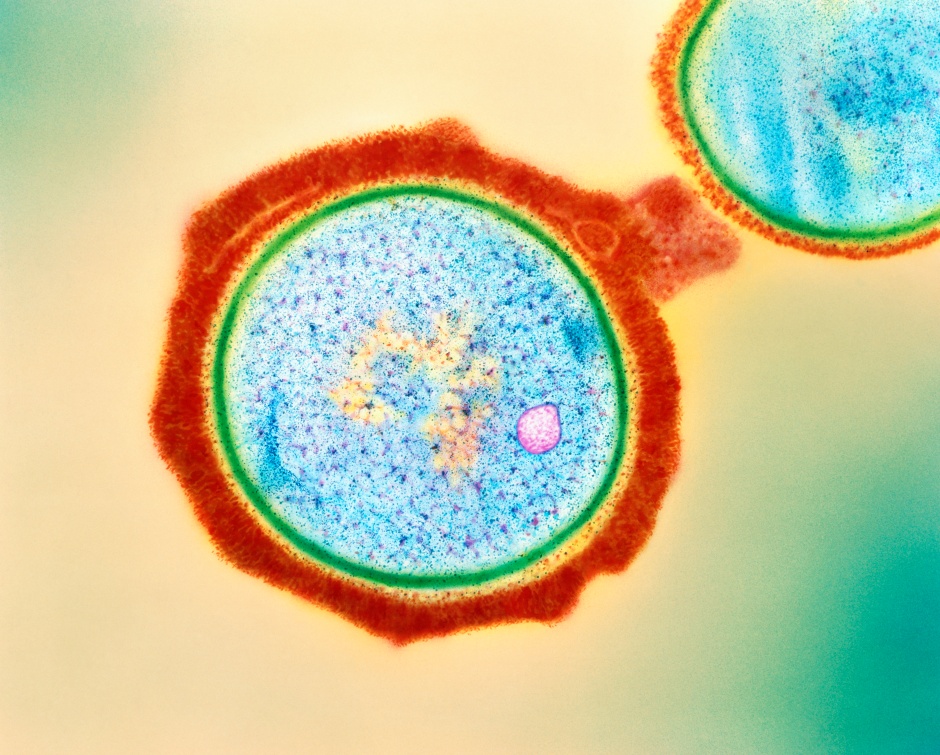
Desmodus rotundus betaherpesvirus (DrBHV) is a nonpathogenic herpes virus that can only infect vampire bats and closely related bat species. Researchers recognized that DrBHV could be used to make a transmissible vaccine for bats, but they needed to figure out how effective it might be. To do this, they first made statistical models using sequencing data from bat saliva samples to determine the transmission dynamics of DrBHV. Afterwards, they could estimate how the transmissible vaccine would affect rabies outbreaks. From their simulations, researchers showed that vaccinating a single vampire bat could immunize over 80% of a bat population, reaching herd immunity to rabies. They also found that DrBHV is similar to other herpes viruses and can establish a life-long infection where the virus cycles between dormant and active states. This suggests that a vaccine using DrBHV would not only be transmissible to other bats, but it also could be “self-boosting” as a dormant virus reactivating would also reactive the immune response to rabies. A transmissible vaccine made with DrBHV has the potential to decrease rabies outbreaks by 50 to 95% and would significantly reduce the disease’s impacts on human health. This research study not only offers a solution to combat viral reservoirs but also lays the groundwork for developing other safe and effective transmissible vaccines.
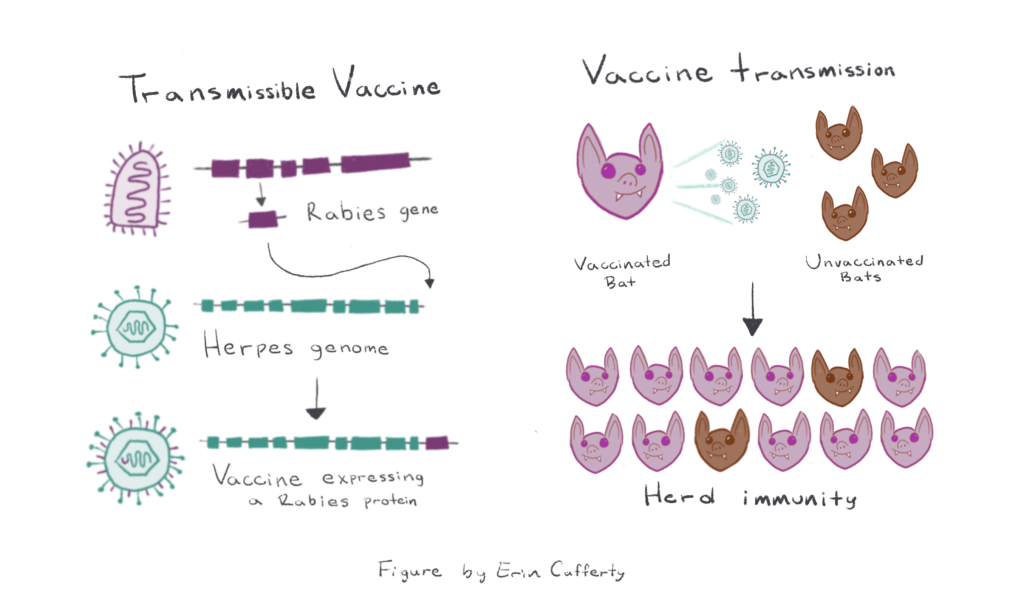
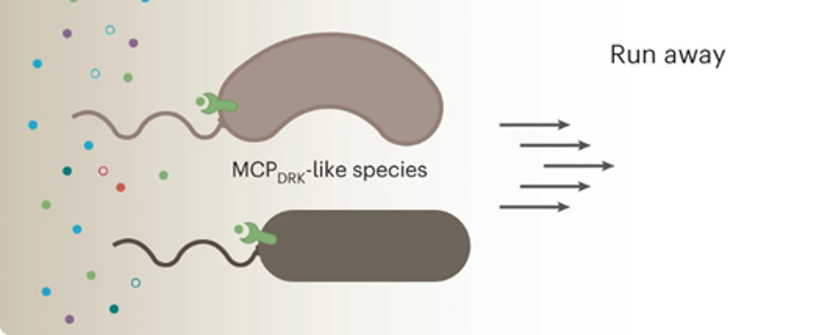
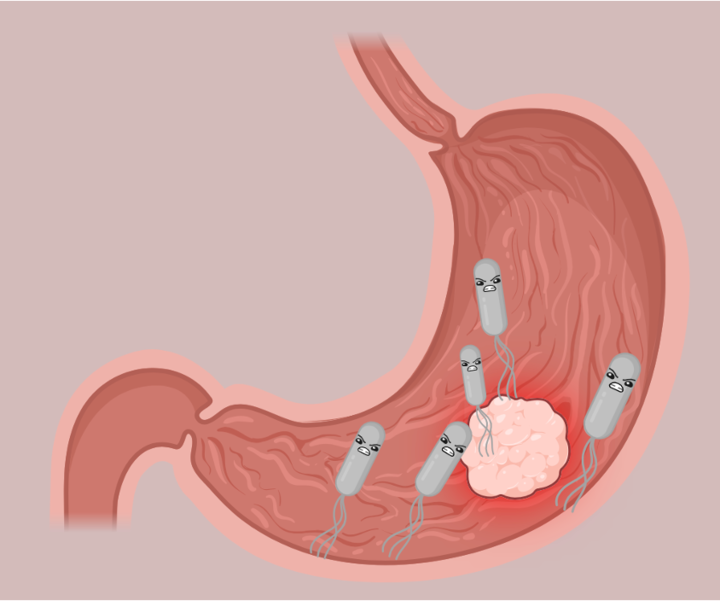
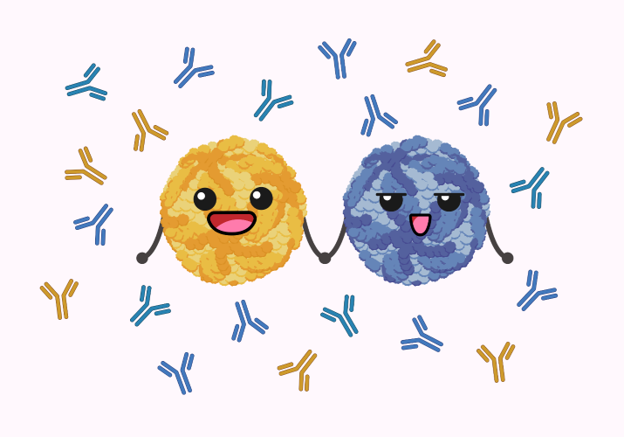
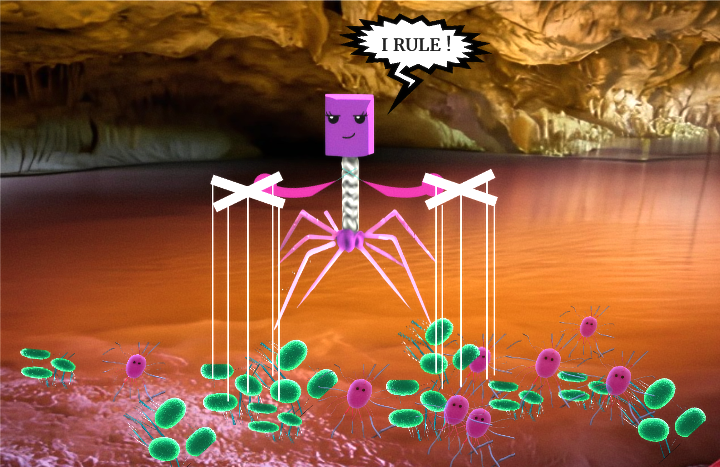
This results in the nonpathogenic Herpes virus expressing a Rabies protein, which is used as the transmissible vaccine (shown in teal and purple).
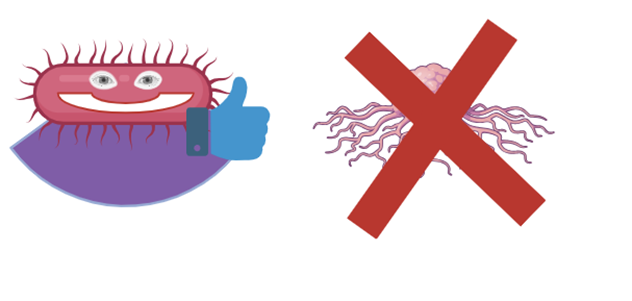
Right: A bat vaccinated with the transmissible vaccine is shown in purple
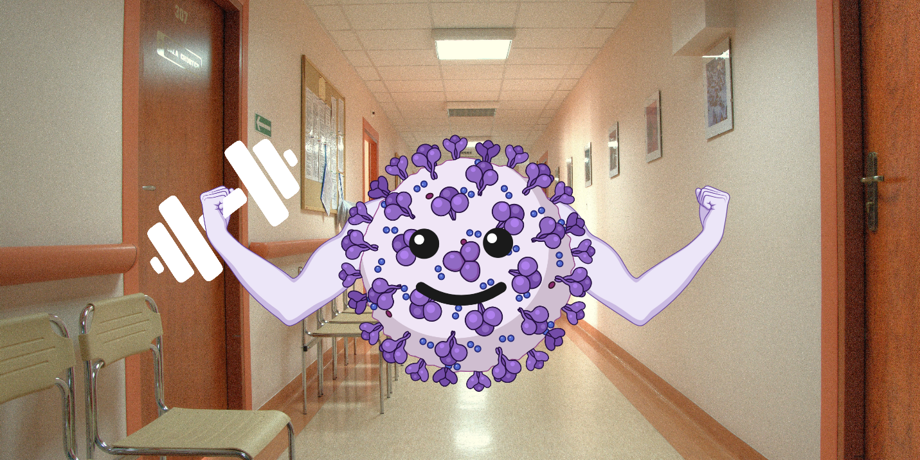
A vaccinated bat (shown in purple) spreads the vaccine virus to unvaccinated bats (shown in brown). Over time, this can lead to herd immunity, where most of the bats in a population are immune to Rabies virus.
Additional sources:
Epidemiology and biology of a herpesvirus in rabies endemic vampire bat populations
Previous research from same authors, https://www.nature.com/articles/s41467-020-19832-4
Featured image: Made by the author