Breaking down the microbiology world one bite at a time
Herpes and Brain: Insights from organoid research
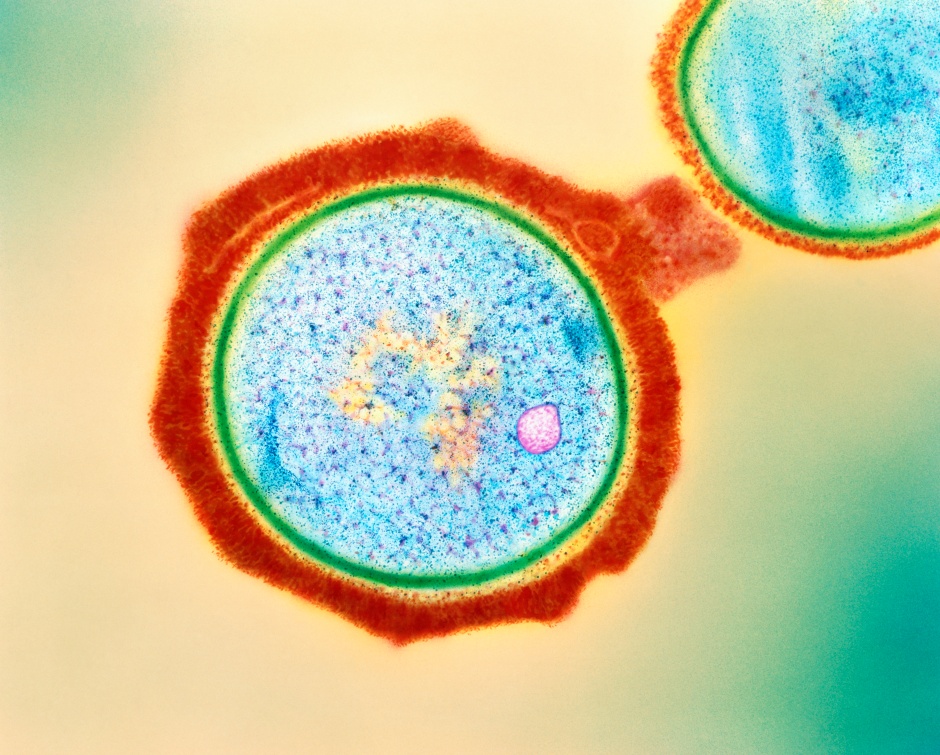
HSV, short for Herpes simplex virus, causes its namesake disease. While Herpes is widely associated with sores around the mouth or genitals, it is not commonly known that Herpes Simplex Virus causes cerebral encephalitis (inflammation of the brain with symptoms like seizures and headache among others).
HSV-1, one of the two subtypes of HSV, infection is treated with an antiviral acyclovir (ACV) which helps to stop the viral replication. However, many individuals experience some neurological consequences after HSV-1 infection due to the damage to neuronal processes and neuroepithelium.
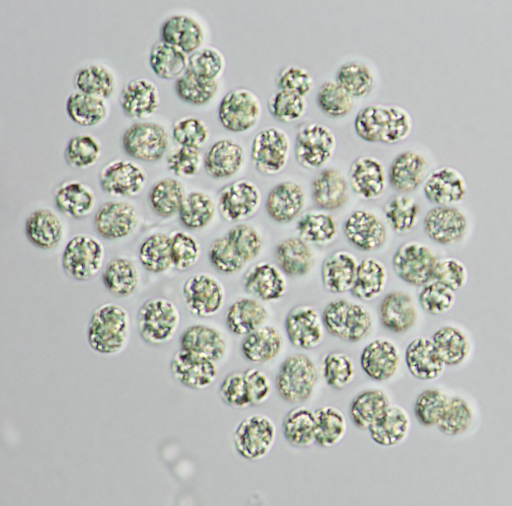
In this study, Rybak-Wolf and their team aimed to better understand the progression of HSV-1 using cerebral organoids, and the effects of antiviral and anti-inflammatory treatment on the cerebral damage caused by HSV-1 infection. Organoids are essentially simplified versions of actual organs that somewhat behave like organs. They can be informally called tiny-brain, mini-liver and so on. This study gave an insight into the association of HSV-1 with brain tissues.
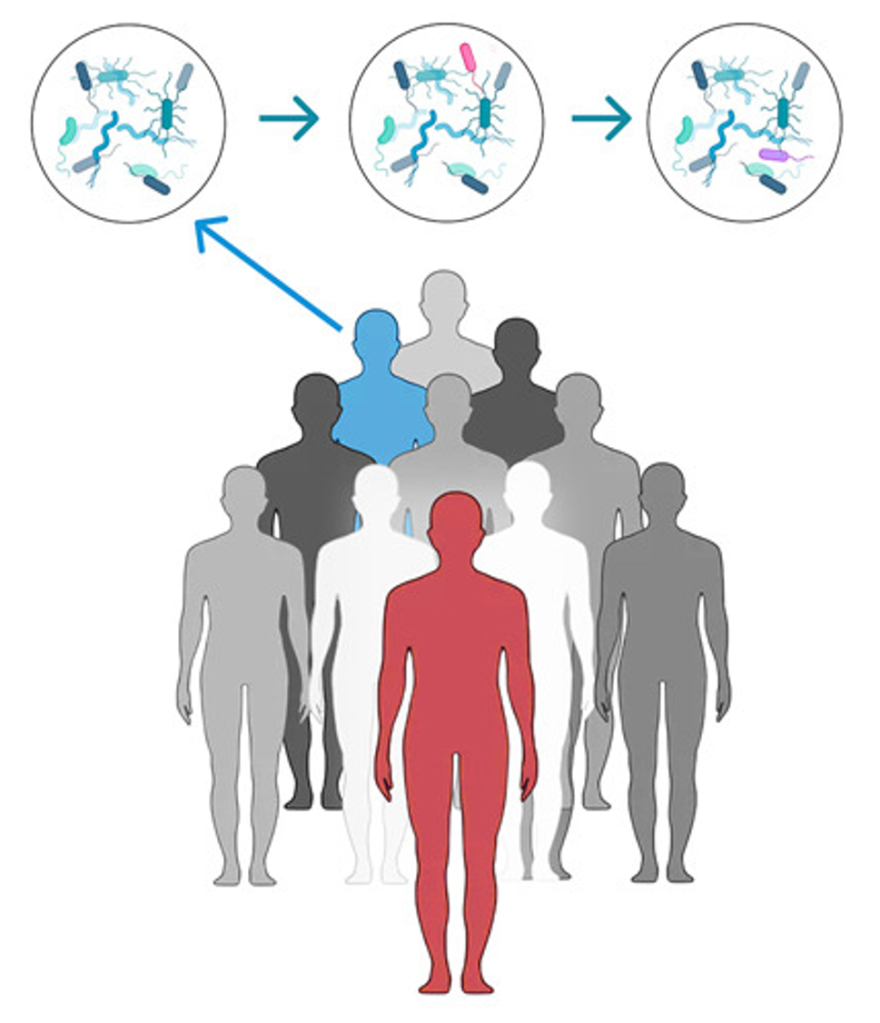
HSV-1 infection is quite common and affects a large part of the population. HSV-1 spreads through close contact like kissing, while the other subtype, HSV-2 usually spreads via sexual contact. This study was centred around the HSV-1 subtype since it is associated with the majority of herpes-associated encephalitis. HSV-1 primarily infects epithelial cells but it can lay dormant in the terminal ganglion region of the brain for decades until it is reactivated by triggers like weakened immunity and stress signals including sun exposure, menses, psychological stress, fever, and surgery. Reactivation can result in the development of Herpes simplex encephalitis (HSE).
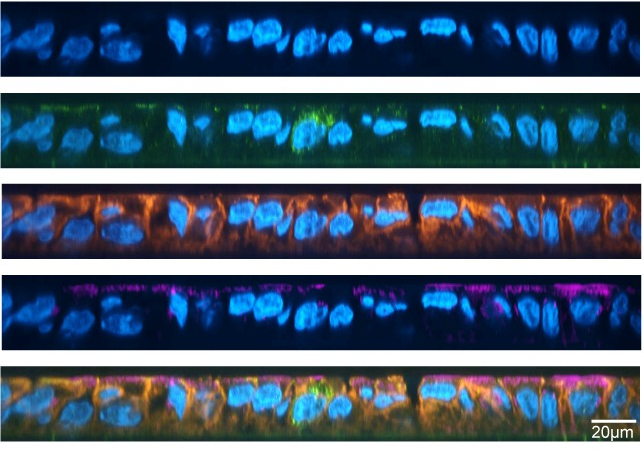
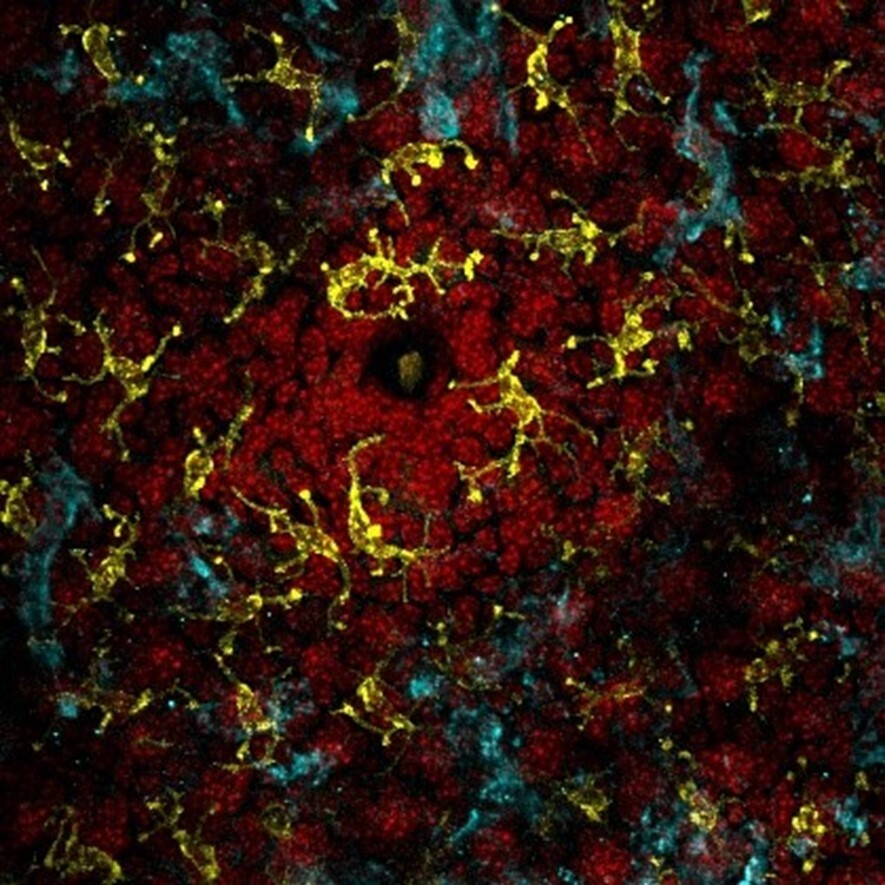
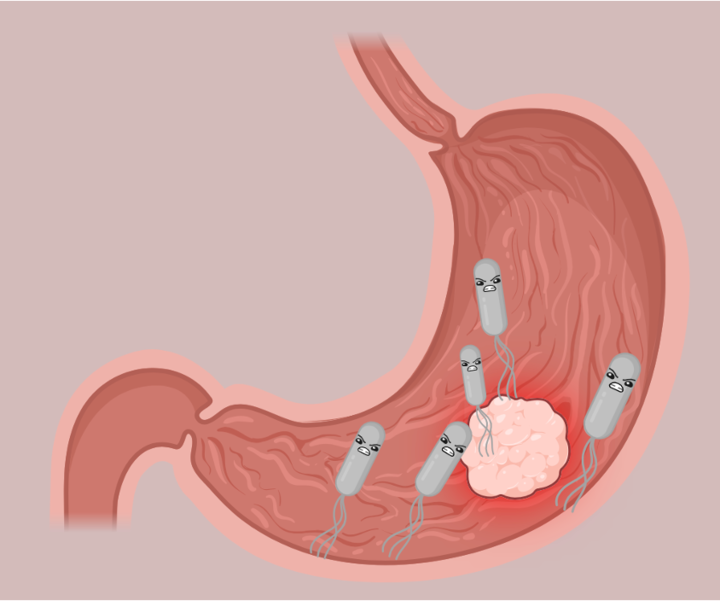
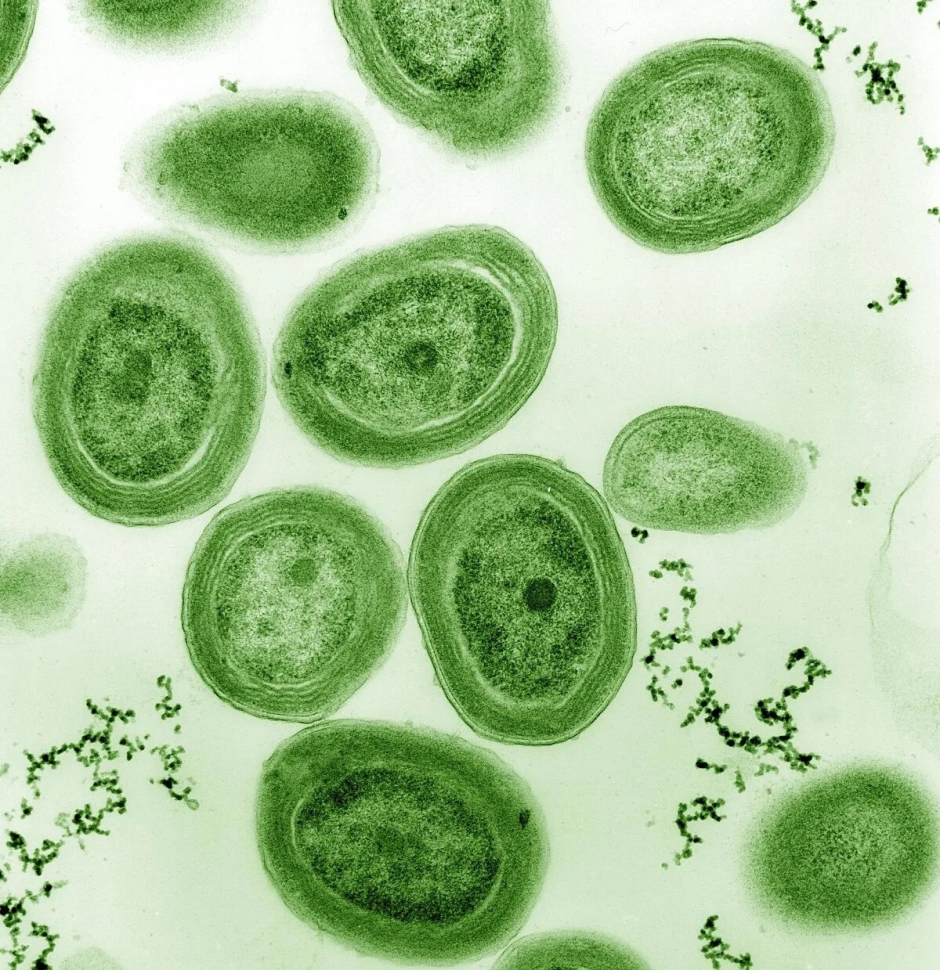
In the study, human brain organoids were created using induced pluripotent stem cell lines (iPS cell line), mimicking the dorsal forebrain. 60-day-old organoids were infected with a fluorescent protein-expressing HIV-1 strain to map the viral spread and analyse cellular and molecular level harm. Researchers also observed changes in cellular identities and expression of several genes and proteins (like SYN1 and HOMER1). Additionally, they measured functional impairment i.e. loss of active neurites as concluded by imaging intracellular calcium since calcium is essential for transmission of signals between neurites. Results from all these tests and analyses point that HSV-1 causes molecular-level impairments, neuronal damage and speedy modifications in neuronal function. Researchers also concluded that inflammation caused by immune response to HSV-1 infection plays a role in damage caused to the brain.

Source– Original article (with modifications)
TNF signalling pathway associated with the transcription factor NF-κB was significantly upregulated. TNF is a cytokine, which is a type of signalling molecule that plays a central role in regulating immune responses and inflammation, and NF-κB is a transcription factor that controls the expression of many genes involved in immune responses, inflammation, cell survival, and other cellular processes. TNF triggers activation of various proteins, including kinases. Kinases, in essence, activate NF-κB to bind to specific sites in DNA. This leads to production of proteins involved in inflammation, immune responses, and cell survival. In brief, they observed inflammation of different cell types in the brain organoids which was caused by TNF signalling via NF-κB.

UMAP plot is a visual representation of complex data which is otherwise hard to understand and visualise. Here, each point represents a single cell and different cell types are represented by different colours.
Researchers analysed the effects of antiviral acyclovir (ACV) alone and in combination with anti-inflammatory drugs (necrostatin-1 and CDDO-Me). They observed that treatment with acyclovir resulted in a significant decrease in HSV-1 replication but failed to stop inflammation. Contrary to this, a combinatorial treatment of acyclovir and anti-inflammatory drugs like necrostatin-1 or CDDO-Me, effectively reduced inflammation.
This study displays evidence to support that brain organoids serve as powerful tools to study invasive viruses and model therapeutic treatments. Limitations of cerebral organoids are that they resemble foetal brains more than adult brains, lack of immune cells and blood vessel supply. While animal models and 2D cultures are useful and have their own set of advantages, they are also limited in their abilities to be effectively used for modelling HSV-1.
We hope that, in the future, more complex human organoids will be created to better understand such infections.
Link to the original post:
Modelling viral encephalitis caused by herpes simplex virus 1 infection in cerebral organoids. Rybak-Wolf, A., Wyler, E., Pentimalli, T.M. et al. Modelling viral encephalitis caused by herpes simplex virus 1 infection in cerebral organoids. Nat Microbiol 8, 1252–1266 (2023). https://doi.org/10.1038/s41564-023-01405-y
Featured image: created by author using bing image creator and canva