Breaking down the microbiology world one bite at a time
A probiotic cream to treat acne
Everyone was/is/will be a teenager once! Along with the teen years comes acne, annoying and sometimes painful with lesions on the skin. If you are/were a teenager, then you know what I am talking about. If you are too young to be one, then… spoiler alert!!
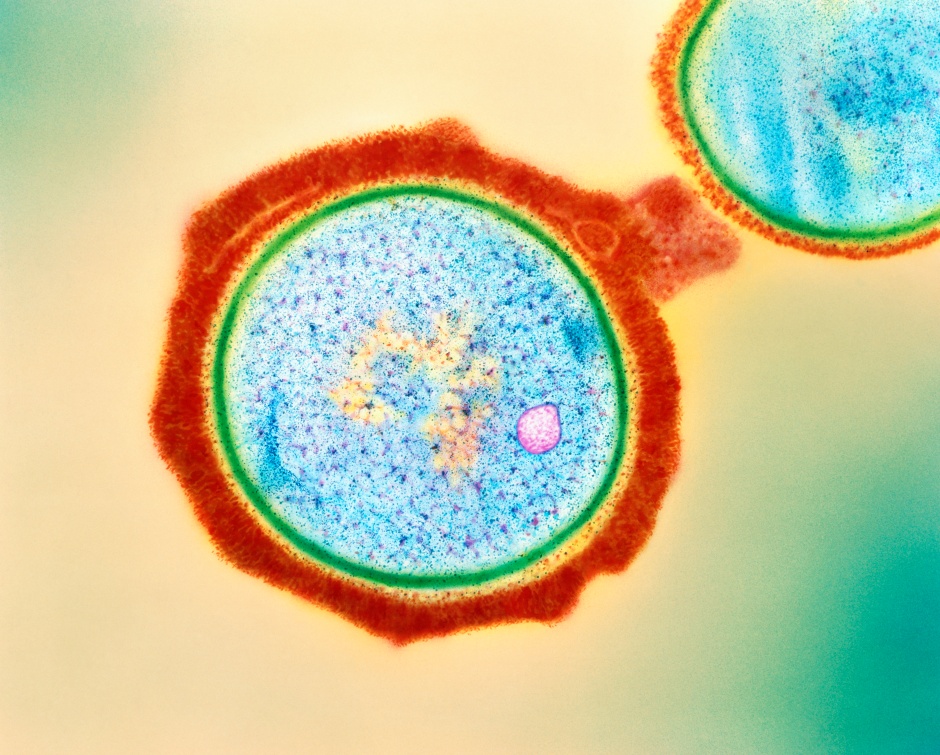
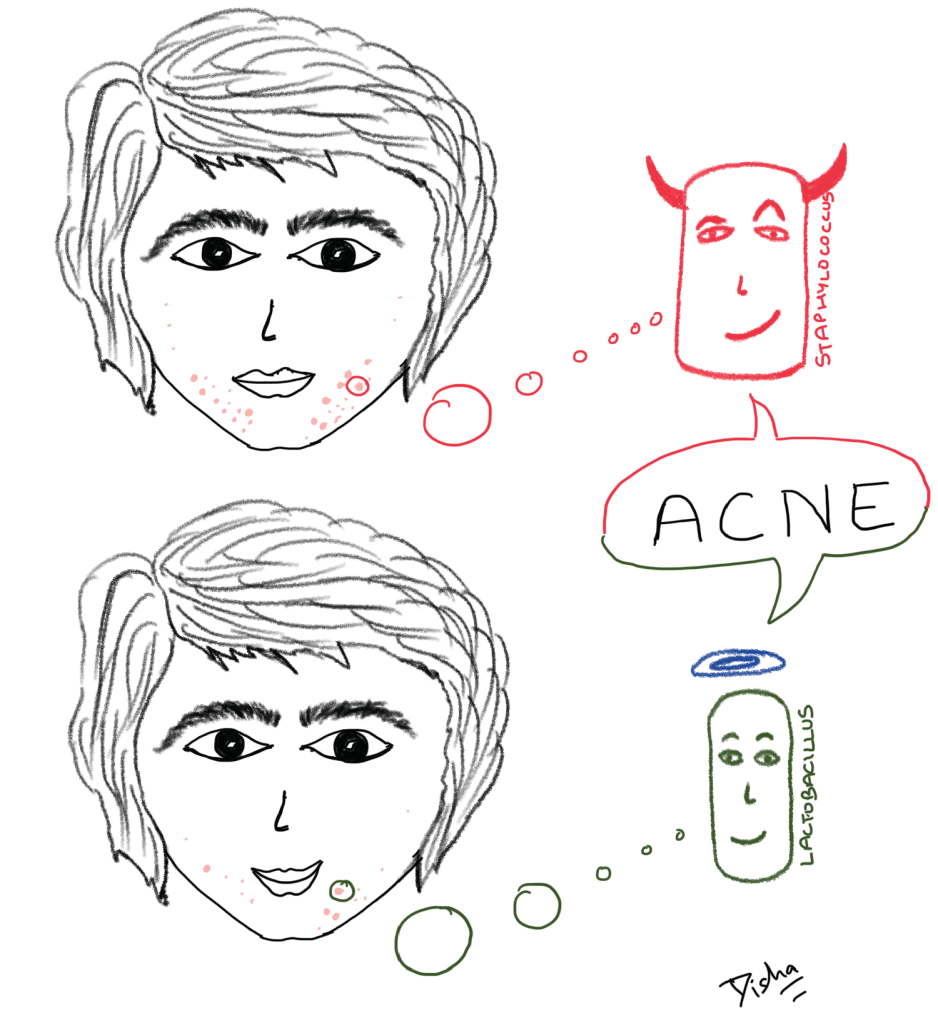
For years, physicians have prescribed antibiotics for acne. Usually, acne are the habitat of Cutibacterium acnes and Staphylococcus aureus. Antibiotics like clindamycin work well against these bacteria, but they come with a tag of… wait for it… you guessed it right: antibiotic resistance. So, the scientists questioned: Is there a way to not use antibiotics and still get the same effect? They found that certain species of Lactobacillus love to combat the bacteria that live in acne.
There are several questions before making Lactobacillus available commercially as a probiotic moisturizer.
Why was Lactobacillus chosen?
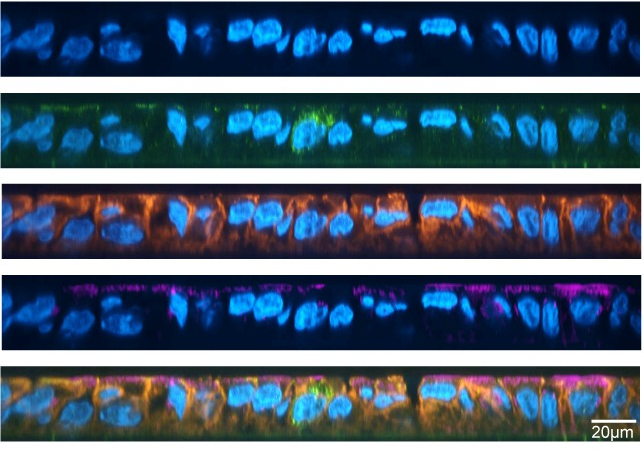
Lactobacillus species are distributed across different sites in the human body, namely, gut, and vagina. Scientific literature provides strong evidence of the beneficial interactions of these species with the other microbes on these sites. For example, in the human gut these bacteria aid in digesting complex polysaccharides, which leads to production of short chain fatty acids. These compounds help in maintaining the integrity of the intestinal barrier because they have an anti-inflammatory effect in the cells lining the intestinal epithelium.
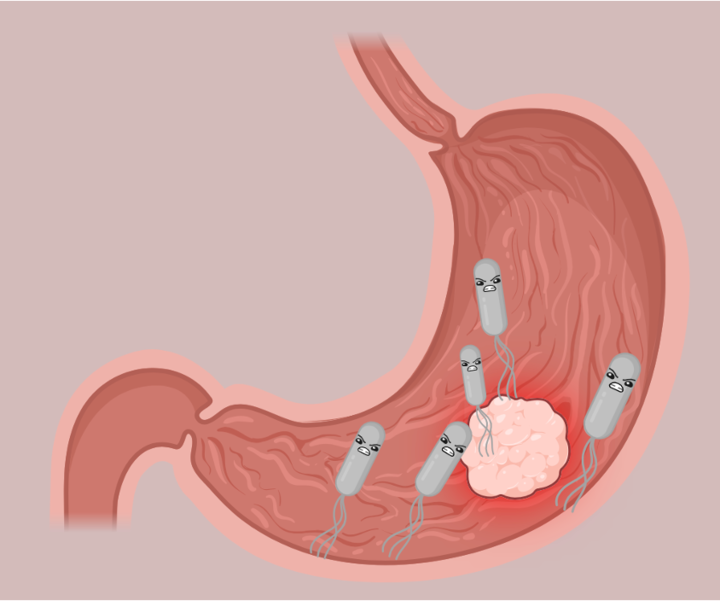
Lactobacillus inhibits the growth of Staphylococcus aureus and also inhibits the activity of lipase enzymes produced by Cutibacterium acnes. Staphylococcus aureus and Cutibacterium acnes cause skin inflammation through different mechanisms. Cutibacterium produces lipase enzymes that metabolize sebum in the acnes to free fatty acids known to cause skin irritation. The mechanism through which Staphylococcus causes inflammation is still not clear.
Spent culture medium is a liquid solution with metabolites released by the microbes after they have reached their optimum growth potential. In this study, researchers tested the growth of Staphylococcus aureus and Cutibacterium acnes in the spent culture media of Lactobacillus rhamnosus, Lactobacillus pentosus and Lactobacillus plantarum amongst other species. They found that all the species inhibited the growth of the two bacteria. In addition, the beneficial Lactobacillus species also inhibited lipase activity of Cutibacterium.
Are these bacteria natural habitants of the skin?
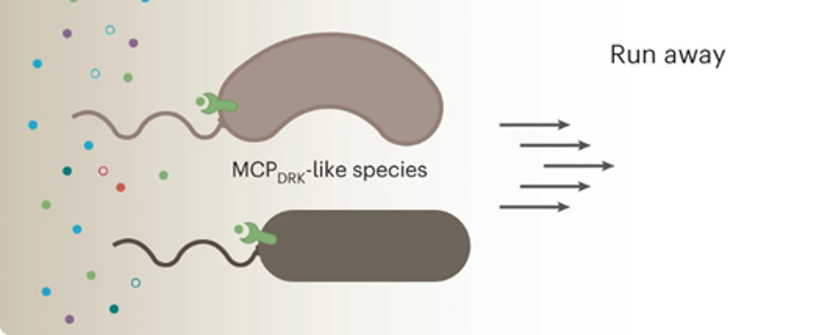
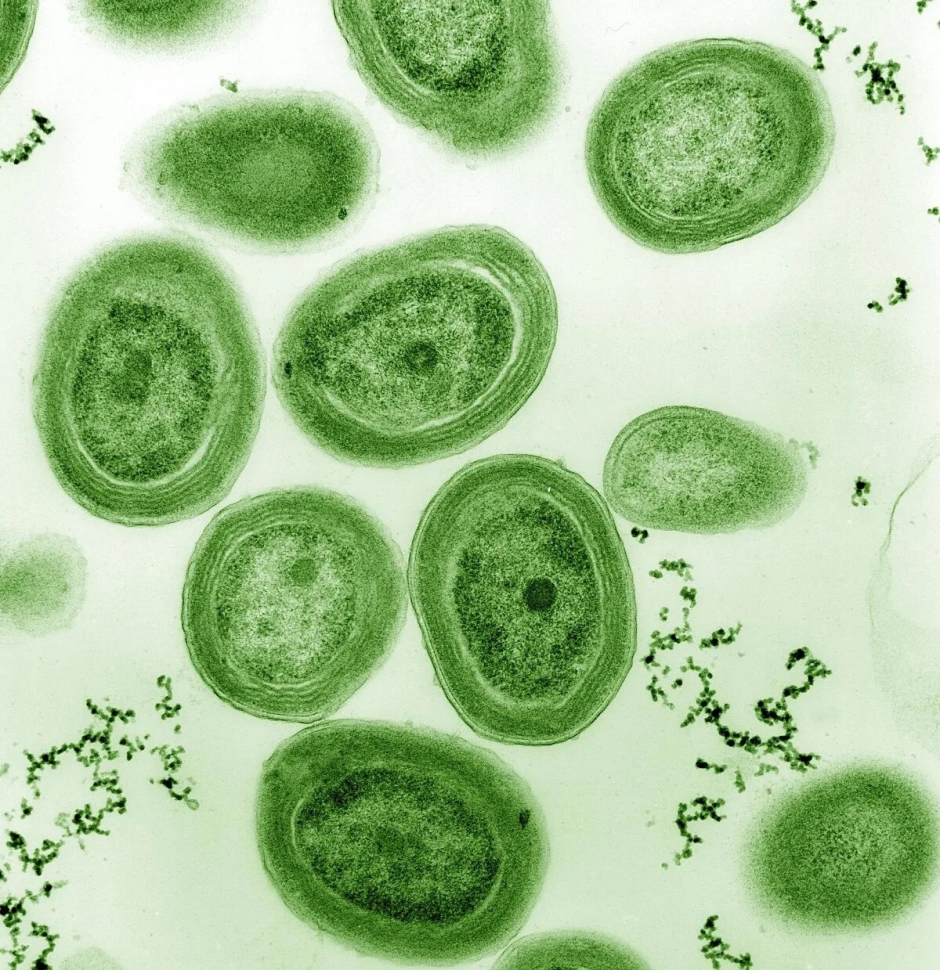
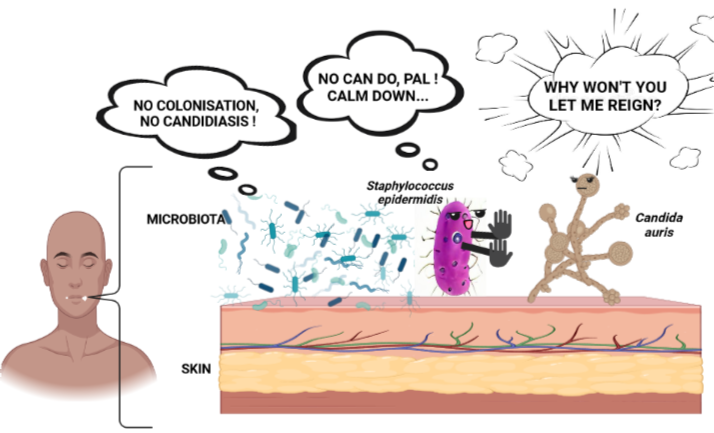
To answer this question, scientists took swabs of cheeks from 30 healthy volunteers (15 male and 15 female) who did not suffer from acne and related skin conditions and tested their microbial composition. They found that Lactobacilli are not amongst the most abundant bacteria on the skin. However, these bacteria still registered their presence in small proportions in most skin samples. Scientists wondered whether this could be a case of contamination. Why? Because facial skin swabs have a very low biomass (meaning that the entire content of the sample does not weigh more than a few milligrams) and could be easily contaminated if volunteers touch their face after touching fermented food products (e.g.: yogurt) or other body sites. The scientists then looked for the presence of Lactobacillus species in publicly available datasets (e.g.: Human Microbiome Project). They found that Lactobacilli are present not only on the face, but also the rest of the skin, albeit in low proportions. This proves that Lactobacillus are no aliens to the skin. But, if that is true, why don’t they already act on the acne? Unfortunately, the number of these bacteria naturally present on the skin are not enough to inhibit the growth of harmful bacteria residing in the acne.
Are these bacteria resistant to antibiotics? Will they come back to haunt us?
Scientists searched for antibiotic resistance genes in the genomes of the selected Lactobacillus species and did not find any. Moreover, according to the guidelines of EFSA (European Food Safety Authority), they tested the effect of the antibiotics on the selected species and did not find any indication of antibiotic resistance.
How does one apply these bacteria to the skin? How do they get dispersed?
We have the bacteria, we know they are safe to use and we know it can protect against invasion of harmful bacteria in acne, but how do we use it? Scientists used two methods: i) freeze-dry the bacteria, encapsulate them in 1.5 -2 mm capsules, mix with the emulsion of oil-in-water cream, or ii) mix the bacteria directly in emulsion, like carrier-in-oil creams (the ones that you get in the usual skin care moisturizers for face-creams). They found that the first approach led to better stability of the bacteria until the time it reaches the skin. When applied with light force, these capsules break and release bacteria on the skin.
A related question is: how safe is the cream? 20 volunteers applied the Lactobacilli-containing capsules to a part of their skin and none of them experienced dryness, rash or swelling.
Efficacy of the cream
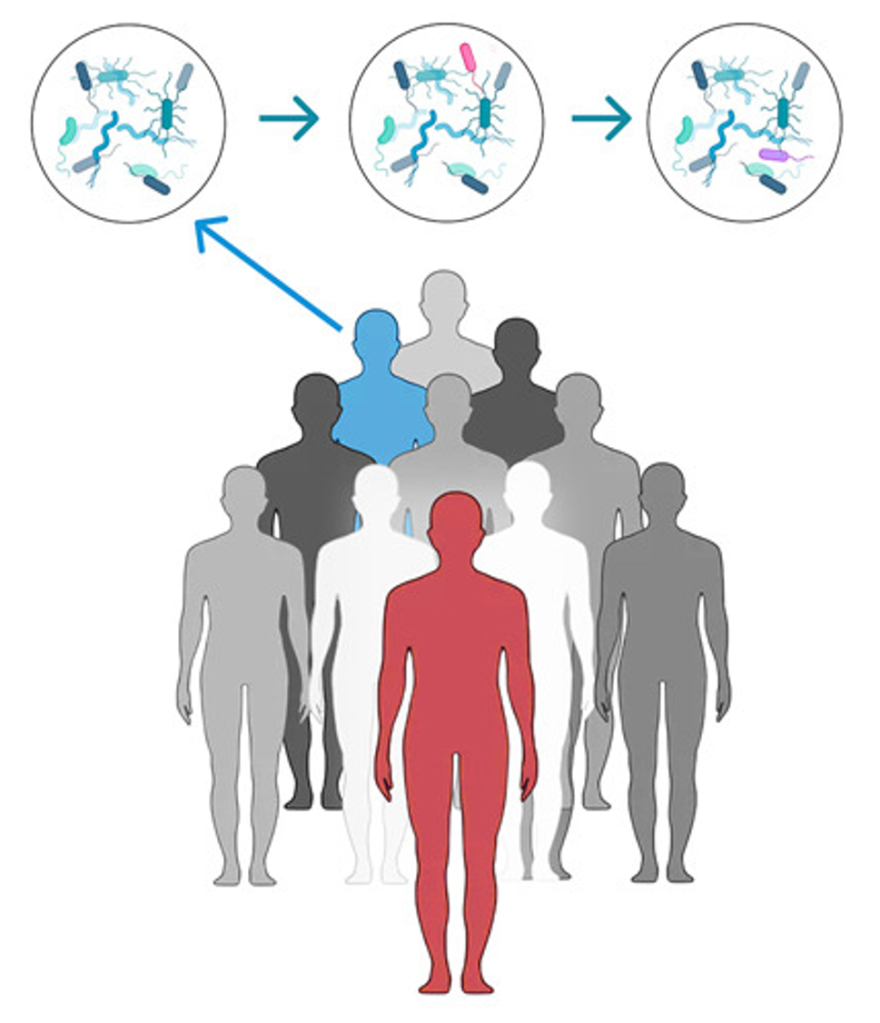
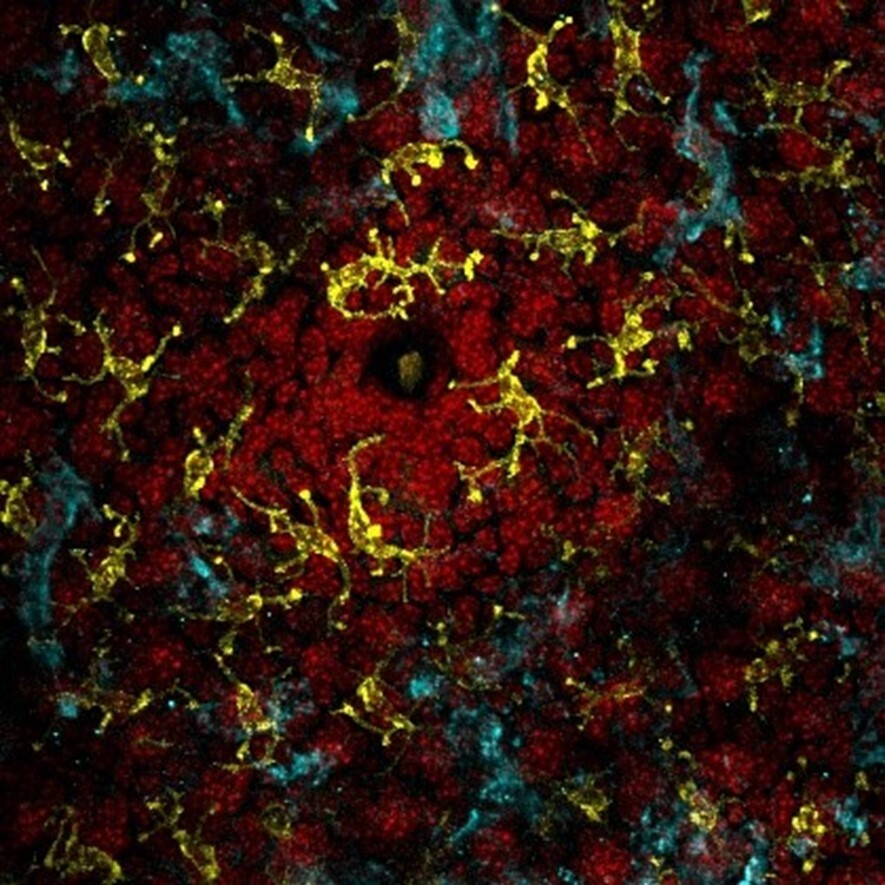
To test the efficacy of the cream, scientists performed a double-blind study with a placebo arm with 79 patients suffering from acne. Double-blind means that neither the patients nor the researchers knew which cream was administered to which patient. All 79 patients had at least 9 inflammatory acne lesions on their skin. Inflammatory lesions mean that acne was painful and appeared like red bumps on the skin. 40 patients applied the Lactobacilli-capsule containing cream (capsule group) and 39 applied placebo cream (placebo group). Skin swabs from patients were taken before, during and after the application. Microbial composition analysis of these samples indicated that there was no disruption of the existing microbial community of the skin for both groups of patients. This means that the otherwise healthy skin microbiome remained healthy even after addition of some new microbes. In the capsule group, there was a statistically significant increase in the relative abundance of Lactobacillus species during the intervention. There was also a statistically significant decrease in the relative abundance of Staphylococcus species during the intervention. This proves the efficacy of the cream with regards to reducing the amount of acne loving bacteria (Figure 1)

There was a significant decrease in the number of inflammatory lesions on the skin of the patients of the capsule group as compared to the placebo group. In addition, the number of inflammatory lesions remained low for the capsule group even after the treatment was stopped. This proves that the capsule cream was effective even with discontinued use.
Future of probiotic cream
This study offers a peek into the huge potential of live bacteria as therapeutic agents for skin conditions. But, this does not mean that you can apply live bacteria directly to your skin. There are methods (like the ones explained in this article) to deliver these bacteria safely to the relevant site. Moreover, extensive research is required to test the efficacy of the beneficial bacteria on different skin types and acne types. Until then, remember that the microbial world has a lot to offer for all aspects of human life, be it delicious fermented food, healthy gut or healthy skin. Stay tuned!
Featured image: Created by author