Breaking down the microbiology world one bite at a time
How do microbes contribute to skin inflammation?
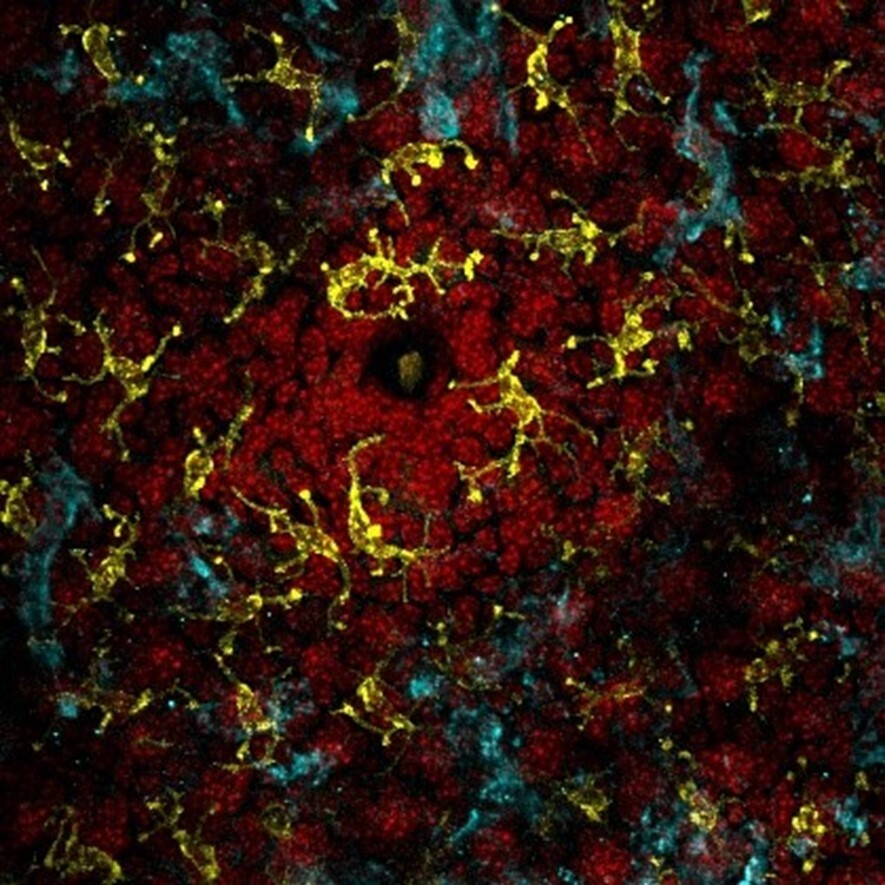
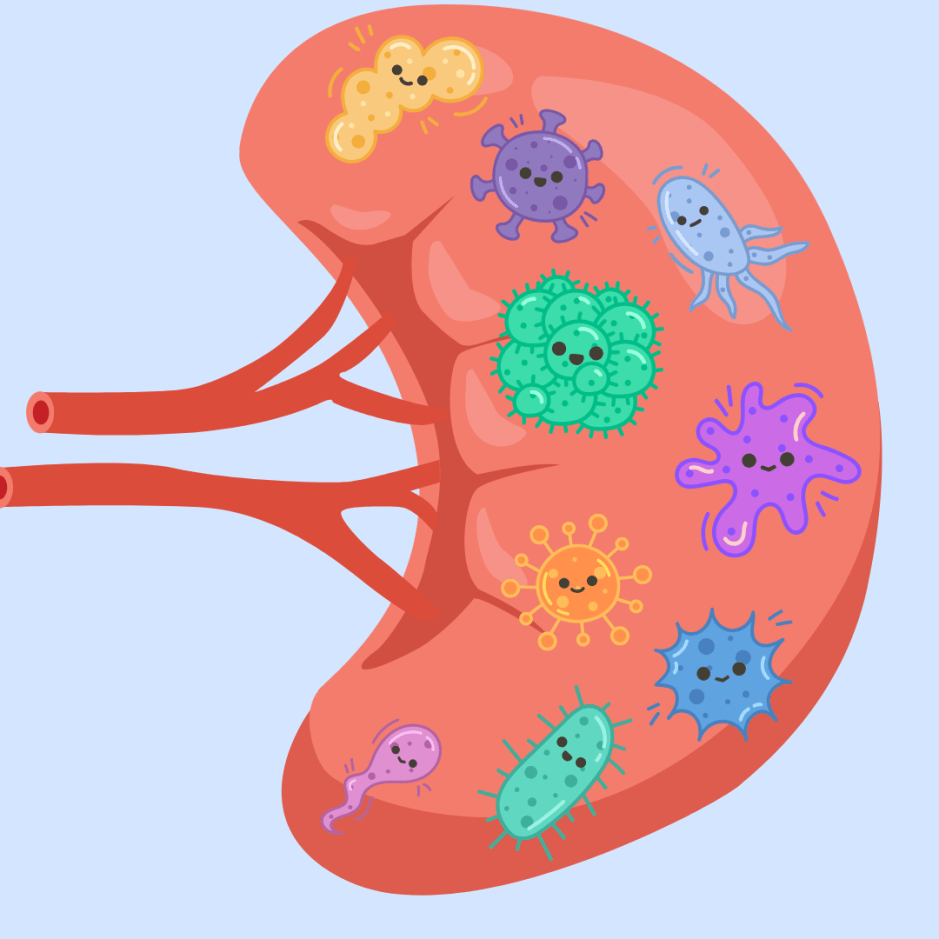
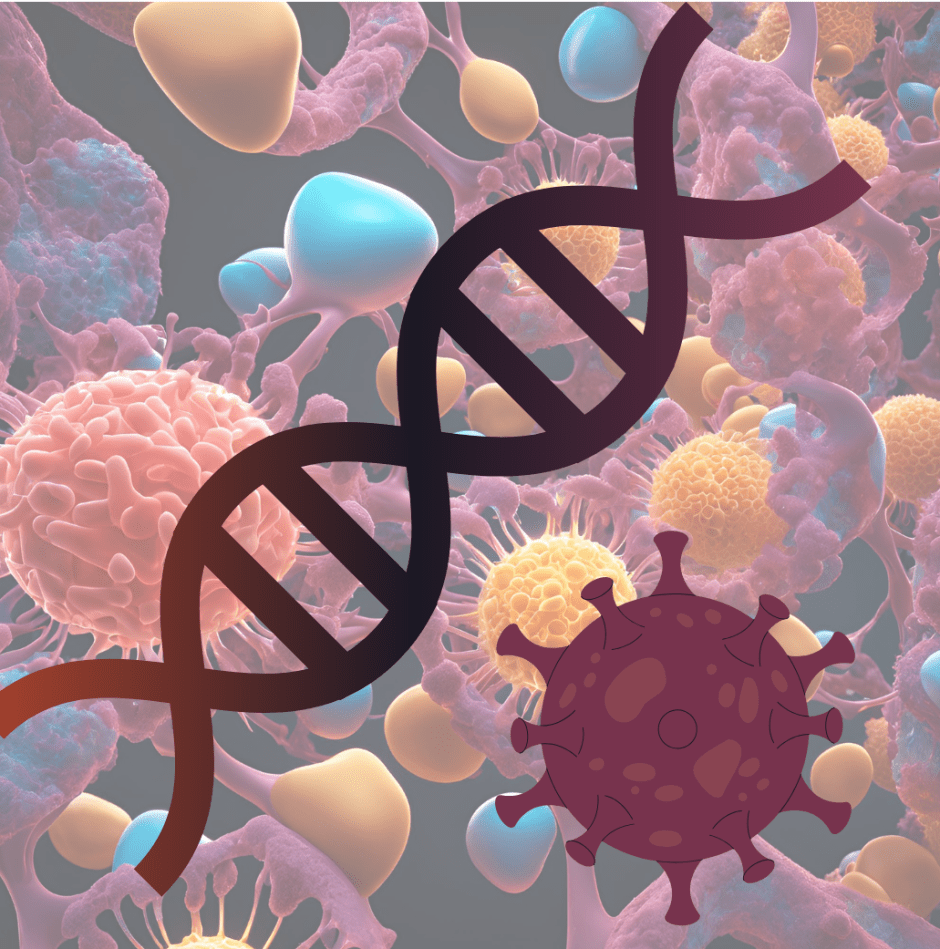
The skin barrier protects our insides from the dangers of the brutal outside world. There is an entire world of microbes living on it. The good microbes on our skin play crucial roles in maintaining regular functioning of the skin such as hair growth as well as promoting wound healing. Curious about what else microbes on your skin can do? The authors of this study definitely were!
In the study, they showed that Staphylococcus lentus on the skin early on influences the extent of inflammation seen in adults by priming (enhancing of cell functioning) a special type of immune cell called the ILC2s.
The authors were interested in understanding why some people exhibit allergic inflammation on the skin and whether this was controlled by microbes. So they ventured into this investigation, which is described below in the following steps.
Step 1: Look at whether known microbes present on skin that help the skin, play any role in inducing dermatitis like inflammation.
Using germ-free mice (a model organism free of microbes) they saw that these mice had lower inflammation than regular mice with microbes, indicating that the microbes can be harmful.
But how?
Step 2: Look at what molecules and cells differ in behaviour when the microbes are absent.
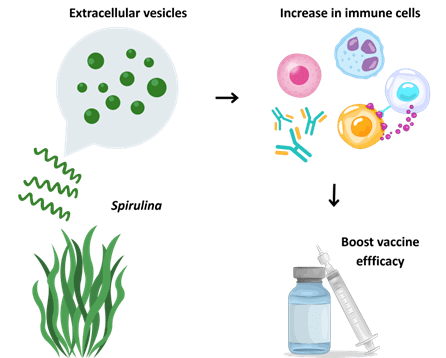
They saw that this specialized type of immune cell called the innate lymphoid cell 2 (ILC2) differed between the germ-free mice and regular mice. ILC2 bridges the adaptive and innate immune system, is capable of secreting chemical molecules that act as a messenger for other cells, and recruiting help for the immune system to fight off invasions.
Why are the ILC2 cells different?
Step 3: Look at how ILC2s react to microbes
The authors took regular mice, depleted microbes on their skin and observed if these cells changed their behaviour. They didn’t see any change. Microbes only influence ILC2 in early life. When no microbes are present, their behaviour is altered, but in adult mice transient depletion doesn’t affect ILC2s.
What does this mean?
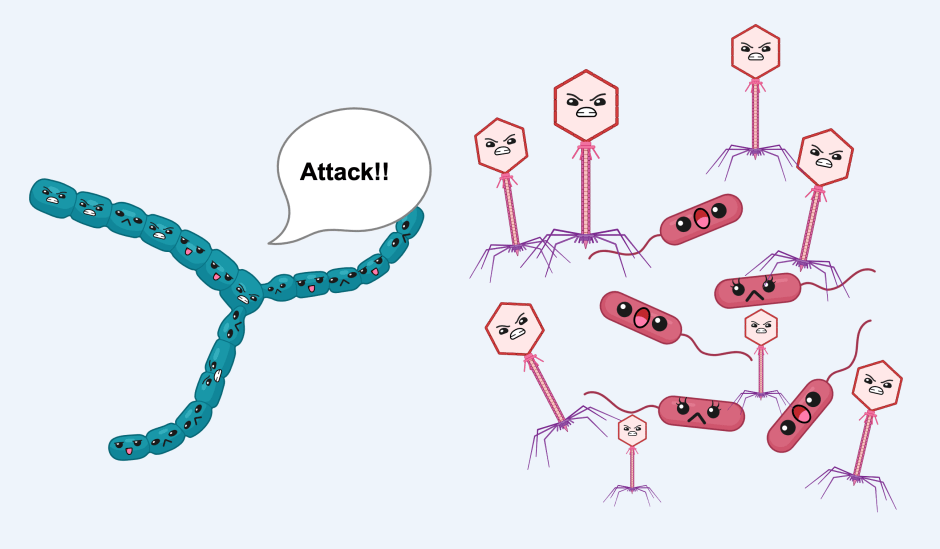
When going to battle, you prepare for it. At least your immune system does! When you have microbes on your skin, the immune system recognizes them foreign and uses them to prepare its soldiers (here ILC2) for battle – priming them. If these microbes ever try to invade into the human kingdom, the soldiers can shoot them down (with dangerous chemical molecules called effector cytokines). And this is something done quite early on during the preparation for war.
If there are no microbes at the later stage, it doesn’t matter. All the soldiers in your army already saw the invaders before and are poised to attack.
Does this mean that the ILC2 knows that the microbes are invaders ? How are they alerted to the microbial presence?
Step 4: Look at how microbes interact with ILC2
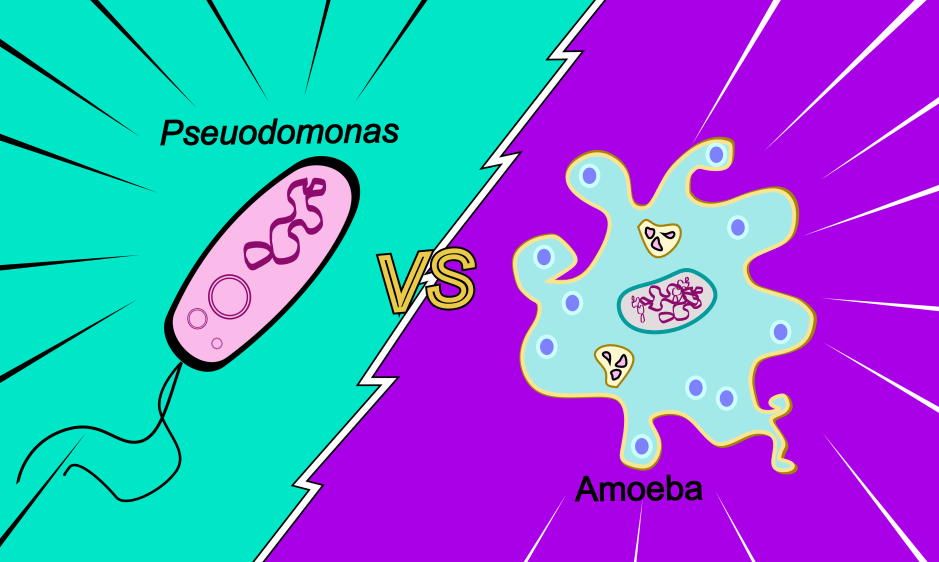
ILC2s interact with chemicals released from other cells in the skin. The group looked at other cells such as keratinocyte (the cell type responsible for making keratin, a protein present in hair, known to interact with microbes). They found that a microbe (later on identified to be Staphylococcus lentus) induces the expression of a protein called thymic stromal lymphopoietin (TSLP) . This TSLP is recognized by ILC2 and initiates a signalling pathway that is equivalent to soldiers preparing for war. One could look at TSLP as a recruiter of soldiers to prepare for war.

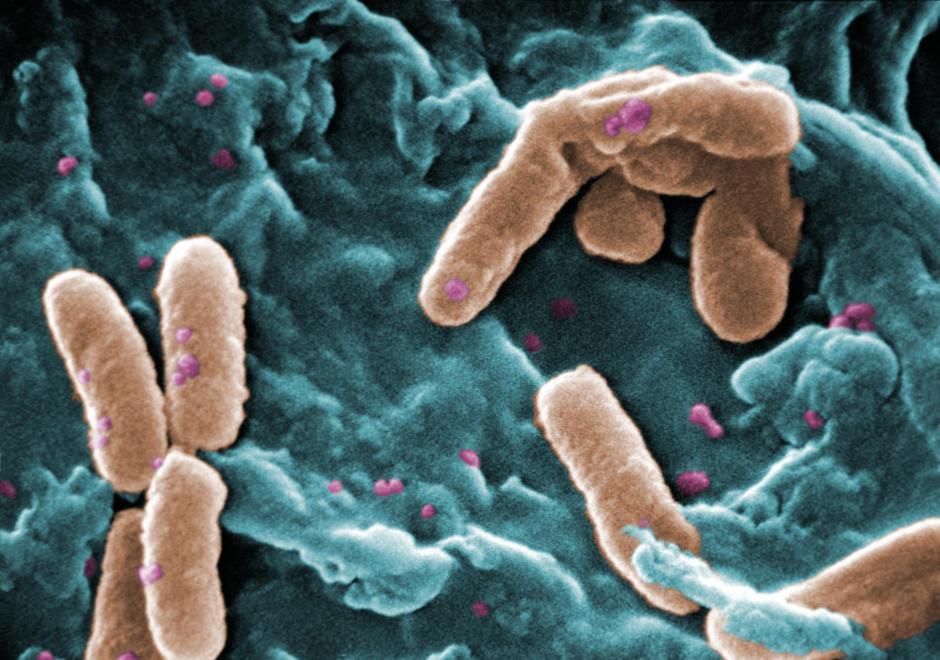
Not all microbes can do this. Here the authors conducted experiments on the microbe that triggered TSLP production by keratinocytes and determined that to be Staphylococcus lentus.
Okay but how does the keratinocyte recognize this bacterium specifically?
Step 5: Look at what is produced by this bacterium.
The authors found that this bacterium produces tryptophan (an amino acid) that signals the keratinocyte to produce TSLP.
That’s all great that the immune system is preparing to go to battle invaders but why does it cause inflammation in adults?
Step 6: Look at adult mice and the keratinocytes there
Observing the enemy early on leads the keratinocyte to constantly produce TSLP which acts as a constant signal to recruit and train more soldiers (ILC2s). Now there are several soldiers ready to pounce. At the first sign of danger, they all start to fight resulting in dermatitis-like inflammation.
Isn’t the human body amazing?! So are these microbes! Today we looked at this story of how microbes on the skin affect the immune system and its response to insults that result in pathology. We also saw how microbiota temporally regulates in the immune system.
Link to the original post: Cha, J., Kim, T. G., Bhae, E., Gwak, H. J., Ju, Y., Choe, Y. H., … & Ryu, J. H. (2024). Skin microbe-dependent TSLP-ILC2 priming axis in early life is co-opted in allergic inflammation. Cell host & microbe, 32(2), 244-260. DOI: 10.1016/j.chom.2023.12.006
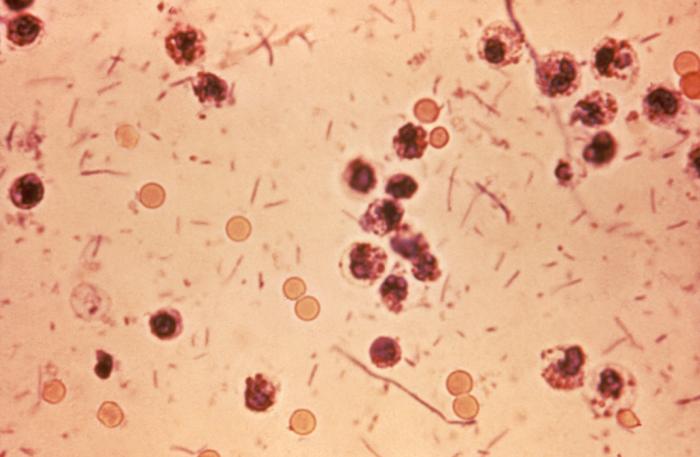
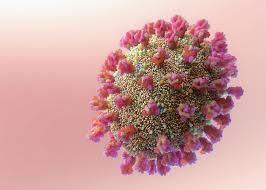
Featured image: Immune cells in the skin NIAID from flickr.com