Breaking down the microbiology world one bite at a time
Diabetic connections lie in our gut
Diabetes plagues 38 million people in the United States, and 1 out of 3 people are prediabetic, marked by an elevated amount of sugar in their bloodstream. The tiny organisms residing in our gut may play a bigger role in the development of diabetes than previously thought. While recent scientific discoveries have made leaps and bounds in finding new ways the gut microbiome plays a role in human health, it was unclear how variation in these microbes can lead to certain people developing diabetes. Researchers at the RIKEN Center for Integrative Medical Sciences in Japan may have uncovered the truth.
Essential to all life is the ability to make energy. Whether that be indirectly from the sun, like plants, or from directly consuming food that was grown and cooked, like a tasty pumpkin pie, breaking down complex nutrients into sugary bits requires a process called glycolysis.
Type-2 diabetes is typically brought on by two different processes. The first is when the pancreas struggles to produce enough insulin, and the second is when our cells and tissues respond poorly to insulin, in a process known as insulin resistance. Normally, the chemical insulin helps get sugar into the muscles and liver so that they can use it for glycolysis. When someone develops insulin resistance, it means that insulin is prevented from doing its job. Eventually, high blood sugar levels can lead to disorders of the circulatory, nervous, and immune systems.
In their recent article, the scientists used human blood and fecal samples from those with insulin resistance, a common marker for prediabetes, and otherwise healthy individuals, to compare differences in gut microbiota.

The researchers first set out to examine the differences in metabolites among these people and found that those with insulin resistance had higher amounts of carbohydrates in their fecal samples, especially monosaccharide sugars like fructose, glucose, and mannose. Complex carbohydrates can be broken down into smaller carbohydrate molecules. They are relatively slow to digest by the human gut, thus keeping in check the blood sugar levels after meals. This makes them ideal for people suffering from insulin resistance. On the contrary, monosaccharides are the smallest carbohydrate molecules. These are digested quickly by the human gut. While providing a quick burst of energy, they can prove harmful to people with insulin resistance because of a sharp rise in their blood sugar levels after meals.
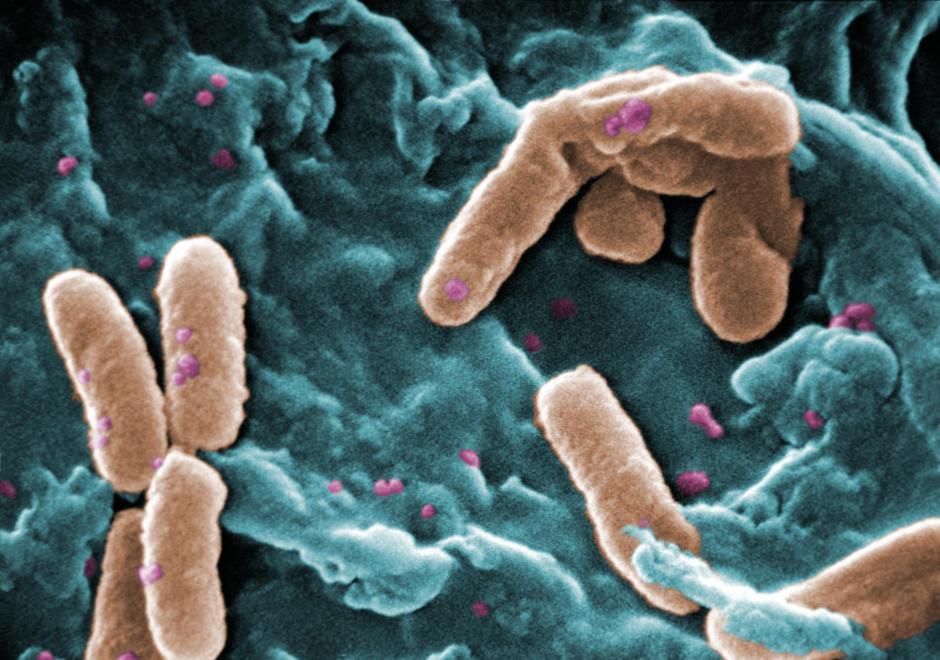
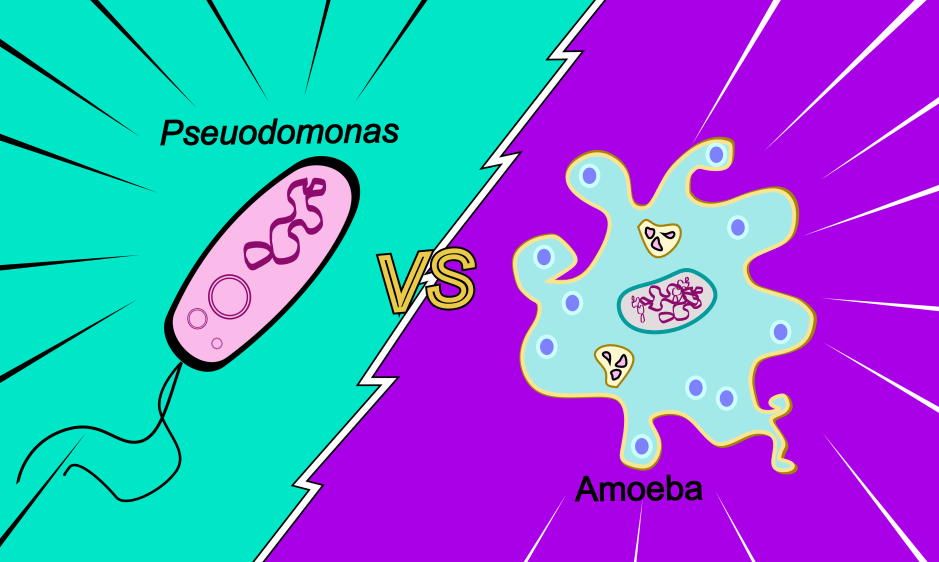
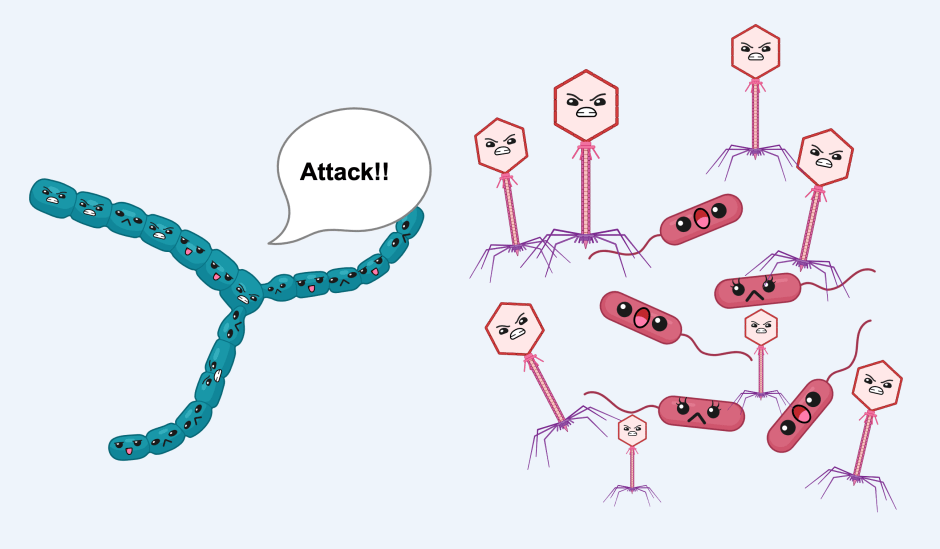
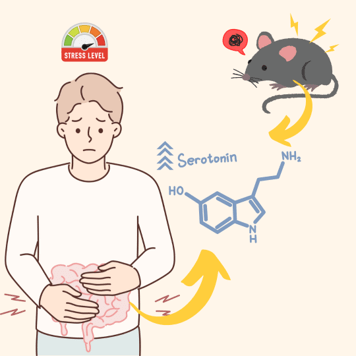
The researchers wondered then if a particular species of bacterium was at play, considering bacteria often have unique metabolisms that create these simple sugars as by-products. Looking at the taxonomic level, the researchers found those with insulin resistance to contain more of the family Lachnospiraceae and this family of bacteria is known to produce high amounts of monosaccharides. In contrast, the participants whose gut contained more Bacteroidales-type bacteria had reduced amounts of these sugars and did not display insulin resistance. If gut bacteria are feeding on these simple sugars, then perhaps this could help people suffering from insulin resistance by making these small sugars unavailable for digestion and hence improve blood sugar levels after meals.
Excited by the prospect, the researchers took to a mouse model to examine the direct effects of bacteria on metabolism. Using an obese mouse model to imitate the diabetic effects, they found that Bacteroidales bacteria, specifically Alistipes indistinctus consumed the same kinds of monosaccharides that were found in the feces of people with high insulin resistance. The idea that there are gut bacteria that can eat and consume these simple sugars, thereby removing them from the bloodstream and cutting the blood sugar levels, poses an interesting way to help those with insulin resistance.
Blood sugar levels were monitored in these mice and the researchers found that A. indistinctus lowered blood sugar, reduced insulin resistance, and the amount of carbohydrates available to the mice.
Senior author and project lead Dr. Hiroshi Ohno shared in a Zoom interview with the author, that the “main target of this project is to identify a gut microbial-related biomarker for prediabetic conditions.”
Because of its association with insulin resistance, the presence of gut Lachnospiraceae bacteria could be a good biomarker for pre-diabetes. Likewise, treatment with probiotics containing A. indistinctus might improve glucose intolerance in those with pre-diabetes.
“So we think we came up with some bacteria that may have clinical effects, but the mechanism underlying those is not very well studied”, said Ohno. “I know the situation in Japan and 1 in 10 of the population is considered pre-diabetic. So, my hope is that in 10 or 20 years the diabetic condition can be decreased.”
Link to the original post: Takeuchi, T., Kubota, T., Nakanishi, Y. et al. Gut microbial carbohydrate metabolism contributes to insulin resistance. Nature 621, 389–395 (2023). https://doi.org/10.1038/s41586-023-06466-x
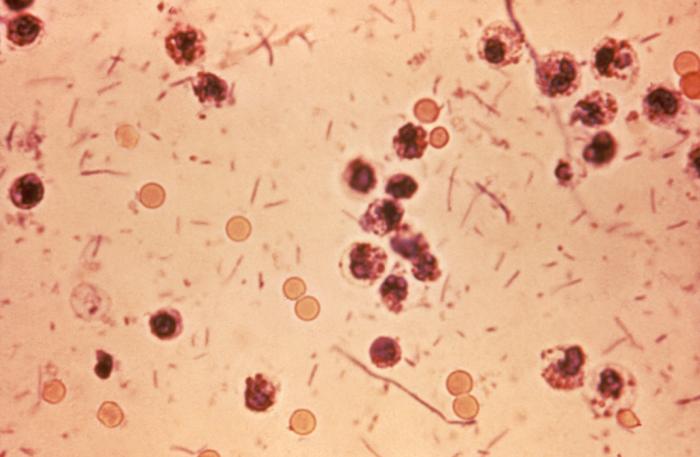
Featured image: Image adapted from flickr. https://www.flickr.com/photos/nihgov/29872812646