Breaking down the microbiology world one bite at a time
Fighting HIV with CRISPR
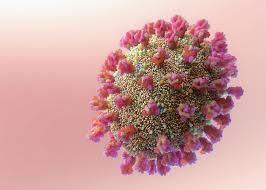
Introduction to HIV
Globally 39 million people were living with HIV infection by the end of 2022, hoping for a cure. Human Immunodeficiency Virus (HIV) destroys our immune system, leaving our body susceptible to various infections and diseases. HIV targets the CD4+ T cells— that is white blood cells (WBC) which help our body in fighting diseases— and destroys them. Currently, antiretroviral therapy or ART is the treatment for HIV infection. ART is a combination of antiretroviral drugs i.e. drugs that work against retrovirus like HIV, namely lamivudine, abacavir and others. While ART increases the life expectancy of HIV-positive individuals and decreases the risk of HIV transmission, it requires a lifelong commitment, therefore, disruption to ART routine can cause rapid return of viruses into the bloodstream since these drugs only work to suppress the virus.
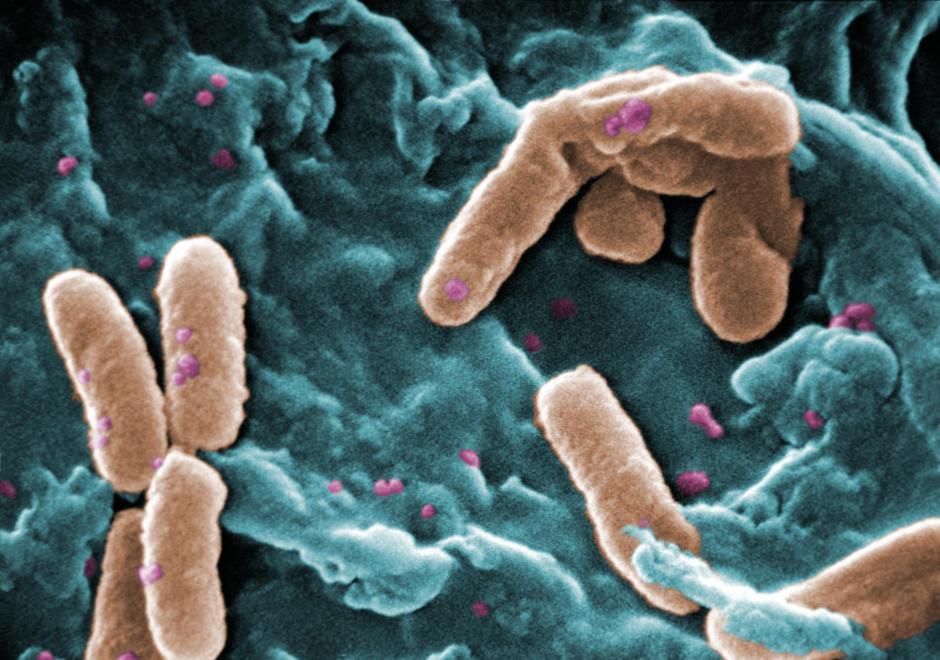
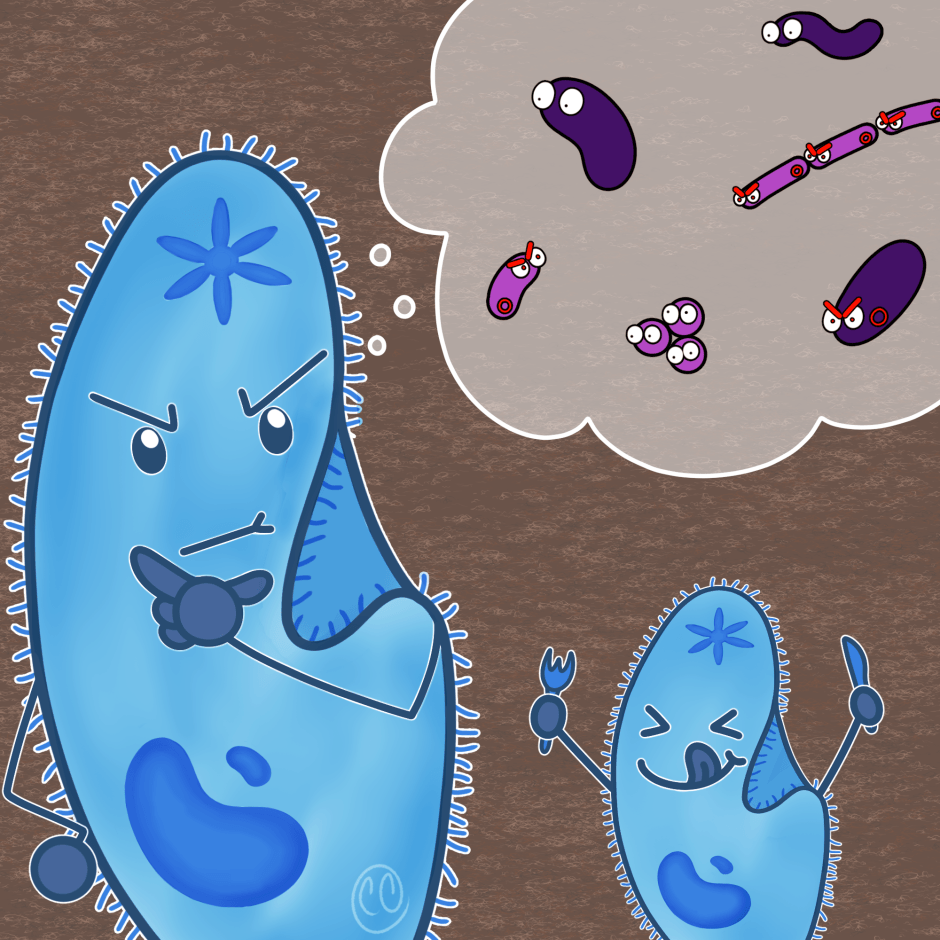
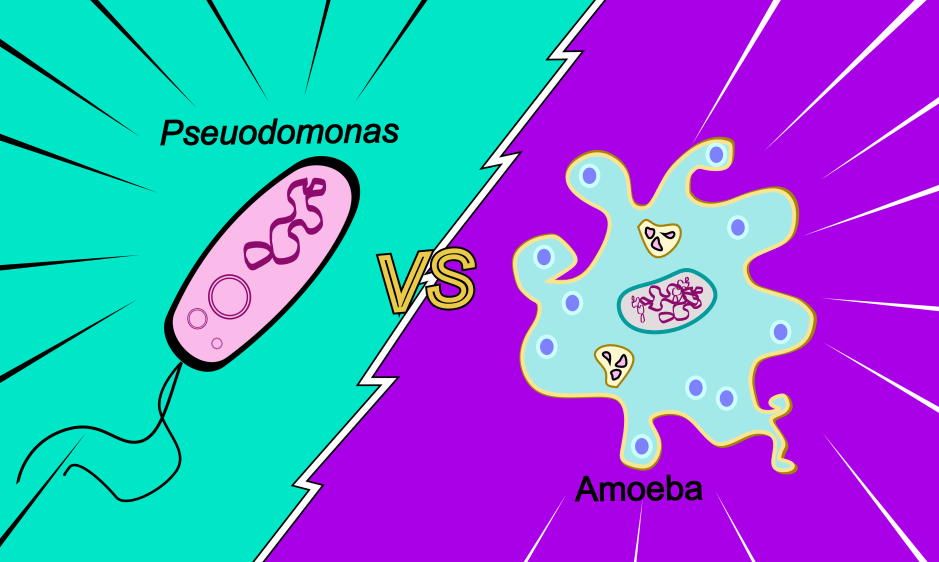
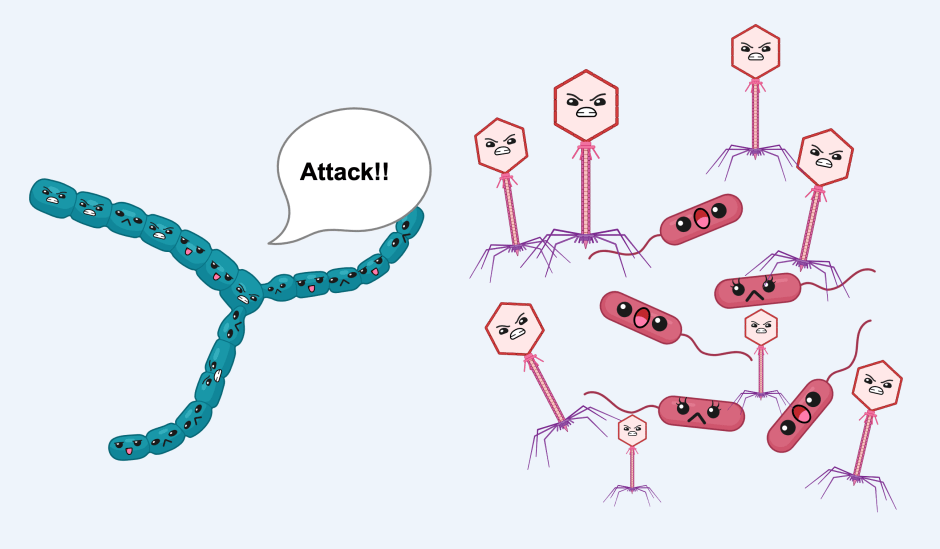
This study explores CRISPR/Cas9 gene editing for the treatment of HIV-1. First, what is CRISPR? It stands for Clustered Regularly Interspaced Short Palindromic Repeats. It is a set of repetitive sequences in bacterial DNA which happen to match viral sequences.Upon viral infection in a bacterial cell, the bacterial DNA sequence is transcribed into RNA, which acts as a ‘guide’ to the Cas enzyme present in bacteria. The Cas enzyme then cuts the viral genetic material, thereby protecting the bacteria from viral infection. This is a naturally occurring mechanism in bacteria and scientists hope to use it for editing targeted genes to treat various diseases in the future.
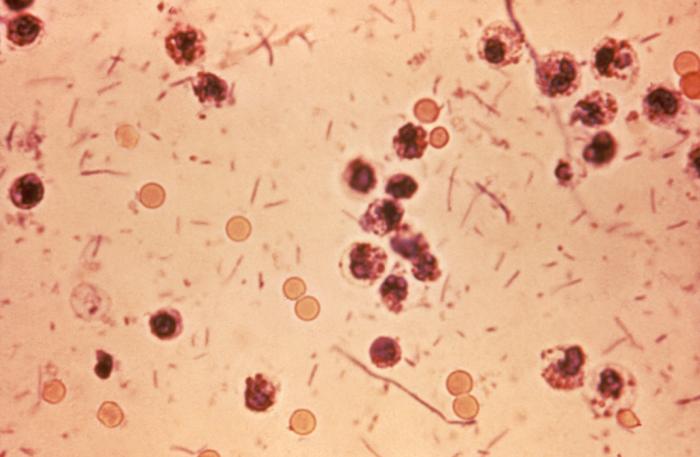
In this study, researchers employed the use of CRISPR/Cas9 for editing the Δ32 allele within the CCR5 gene coding for CCR5 receptors found on CD4+ cells (helper T-cells). HIVs bind to the CCR5 receptors which leads to their entry into CD4+ cells. Upon entering, the HIV makes multiple copies and destroys these cells, causing them to decline in number, eventually, affecting the immune system. The importance of CCR5 receptors in the spread of HIV infection was shown by a study published in 1996. It claimed that the Caucasian participants exhibited a mutation in CCR5 gene which made them considerably resistant to HIV infection. This Δ32 mutation in CCR5 gene was found less frequently in African and Asian participants.
Building upon these findings, researchers of the present study infected humanised mice with HIV-1. To confirm that the mice are infected with HIV, researchers tested them for viral load (amount of virus in the infected body) and the decrease in levels of CD4+ T cells. After successful infection by HIV, they implemented a 3-step treatment routine Starting with ART regimen to suppress the viral infection followed by AAV6 CRISPR/Cas9 (see end of the paragraph for details) for CCR5 gene editing to stop the spreading of the virus, and finally using AAV9 CRISPR/Cas9 to edit LTR-Gag region of HIV to remove proviral DNA fragments. Researchers employed a combination of these therapies on six groups of mice. (Table-1)
AAV6 and AAV9 = Adeno Associated Virus type 6 and 9 are viral vectors used to deliver CRISPR/Cas 9 targeting the CCR5 gene and LTR-Gag region, respectively.
Table-1: Summary of treatments given to each mice group.
| GROUP NUMBER | TREATMENT GIVEN |
|---|---|
| GROUP-1 | No treatment |
| GROUP-2 | CRISPR-Cas9 targeting CCR5 and HIV-1 LTR Gag region |
| GROUP-3 | CAB, 3TC and ABC prodrugs, and RPV i.e ART |
| GROUP-4 | ART regimen + IV injection of AAV9-CRISPR-Cas9-targeting LTR-Gag |
| GROUP-5 | ART regimen + IV injection of AAV6-CRISPR-Cas9-targeting CCR5 |
| GROUP-6 | ART regimen + dual CRISPR (targeting CCR5 and HIV-1 LTR Gag) |
Results
After treatment, each group of mice was tested to establish the efficacy of each treatment. Tests were performed from the spleen, bone marrow, gut, brain, liver, and lung tissues in each mice group.
All the groups treated with ART displayed increased counts of CD4+ T cells. CD4+ levels were moderate in group 4 and group 5, while group 6 displayed the highest number of CD4+ cells. However, the number of CD4+ T cells was the lowest in group 2.
DNA and RNA levels of HIV in mice groups were also evaluated. Group 6 that received ART with dual CRISPR/Cas9 therapy had no viral DNA in their spleen, gut, bone marrow, lung, liver, kidney, and brain.
Various other analyses were performed to validate these results like RNAscope, viral outgrowth assays, and droplet digital PCR. Moreover, researchers also observed no ART or CRISPR-related toxicities by histological (tissue) analyses of spleen, liver, and kidney tissues.

What does it mean?
Dual CRISPR therapy showed significant improvements in HIV-1 cure rates compared to single treatments implying its crucial role in eliminating HIV-1 infection.
Even so this treatment method has its limitations. The virus-carrying system (AAV) is not specific to HIV, which may cause it to miss some latent virus reservoirs in the body. CRISPR-Cas system needs to reach all HIV-infected cells, but it’s not clear how to ensure that happens. Due to non-specific targeting, some latent HIV may not be removed, leading to a rebound of the virus in some of the treated animals.
Despite the limitations, ART with dual CRISPR achieved effective elimination of HIV-1 and has the potential for clinical application.
Link to the original post:
CRISPR editing of CCR5 and HIV-1 facilitates viral elimination in antiretroviral drug-suppressed virus-infected humanized mice. 10.1073/pnas.2217887120 Dash, Prasanta K., et al. “CRISPR editing of CCR5 and HIV-1 facilitates viral elimination in antiretroviral drug-suppressed virus-infected humanized mice.” Proceedings of the National Academy of Sciences 120.19 (2023): e2217887120.
Featured image: Made by author with bioicons and canva
Other References-
Dash PK, Chen C, Kaminski R, et al. CRISPR editing of CCR5 and HIV-1 facilitates viral elimination in antiretroviral drug-suppressed virus-infected humanized mice. Proc Natl Acad Sci U S A. 2023;120(19):e2217887120. doi:10.1073/pnas.2217887120
Abdul A. Waheed and Eric O. Freed. HIV Type 1 Gag as a Target for Antiviral Therapy. AIDS Research and Human Retroviruses.Jan 2012.54-75.http://doi.org/10.1089/aid.2011.0230