Breaking down the microbiology world one bite at a time
How does you falling ill affect the microbes that exist within you?
Thousands of other living species have found their home in various parts of the human body. One such hotspot in the human body is our gut. Interestingly there are more non-human cells in us than humans. And hence, these microbes have a tremendous impact on our lives and health and, in turn, are also impacted by our lives and health. So, a group of scientists from Yale set out to understand how the microbes that found a home within us are affected when we fall ill.
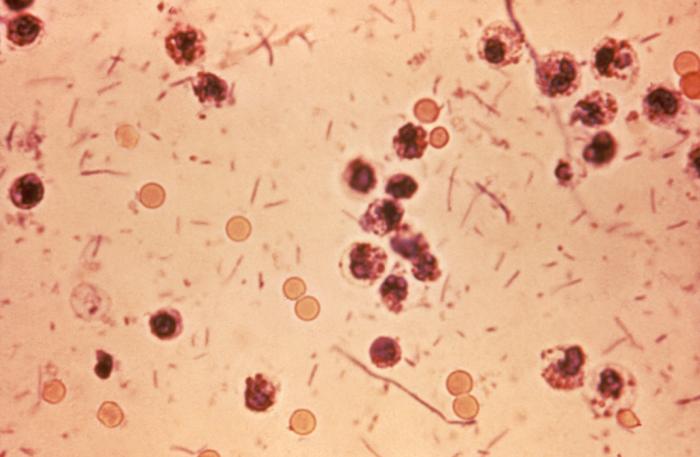
They used mice as their model organism, in particular gnotobiotic mice. Gnotobiotic mice refer to mice reared in a sterile environment to exclude all microorganisms. So gnotobiotic mice would not have their own gut microbe.
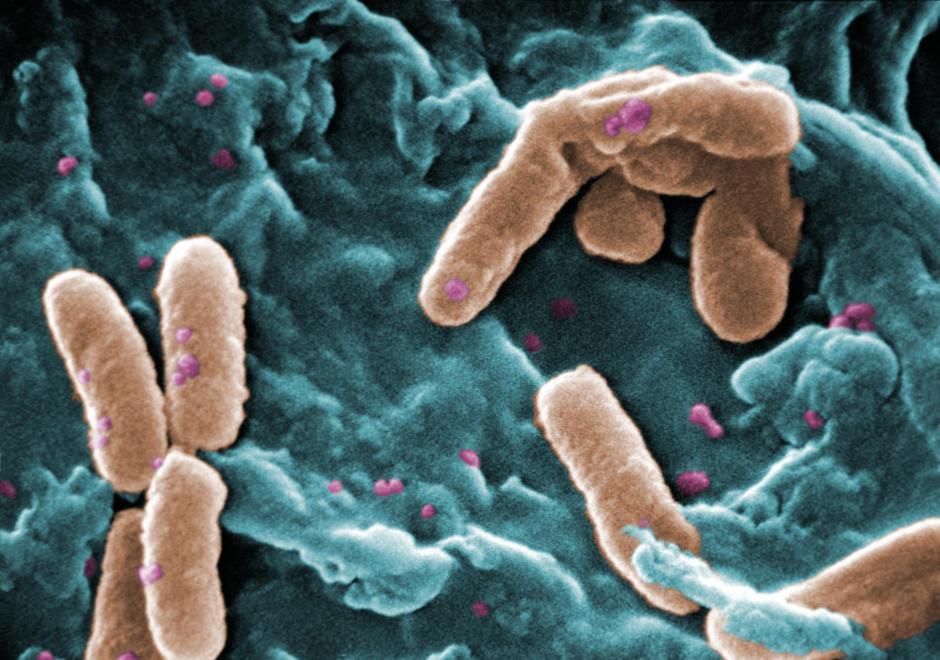
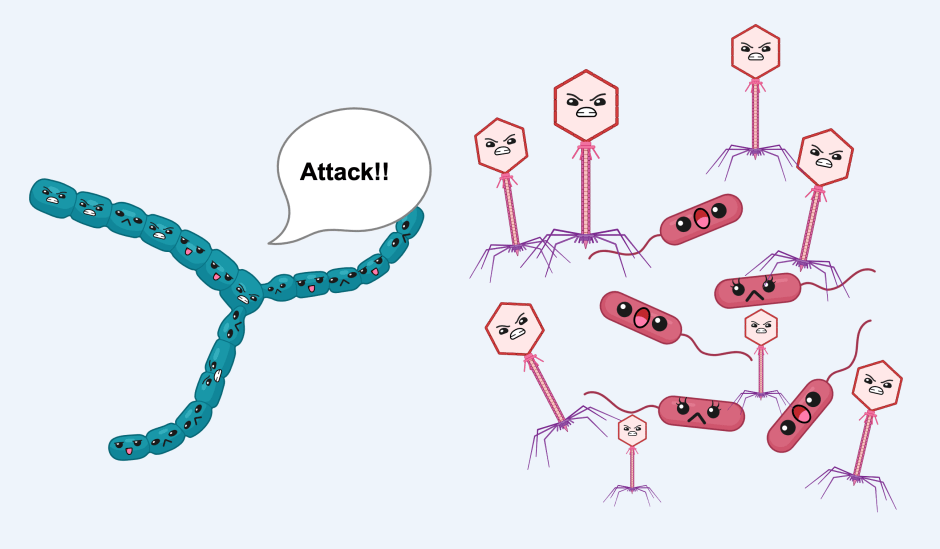
The researchers then artificially introduced different strains (genetically distinct lineages) of the bacteria B. thetaiotamicron into gnotobiotic mice and saw that the different populations were stable under normal conditions (homeostasis) however, undergoes changes when infected with a pathogen, that is a dangerous microbe, C. rodentium. When infected with the bug, some of the strains selectively expand rapidly and dominate the B. thetaiotamicron population.
Just like when someone moves to a new house, they adapt themselves to their new neighbourhood and adjust to their new commute; microbes also do the same in their hosts. The study found that B. thetaiotamicron populations adapted to the mice’s gut, and the nature of the adaptation differed based on whether the mouse was healthy or infected.
Upon further investigation, they observed that a dominant strain in the infected mice had identical single point mutations. Point mutation refers to a single base pair change in the genome; it can be compared to if a single note was altered in a musical composition. This mutation resulted in the production of an altered protein meaning that the genome encodes information that is relevant for protein production in the bacteria, which allows it to grow better in the infected mice’s intestines.
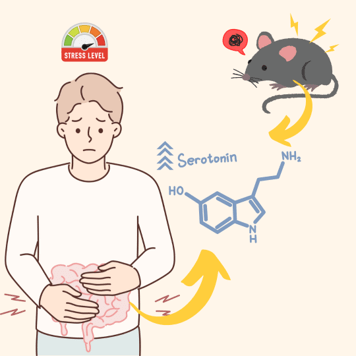
What is the role of this protein, and how is it making the bacterial strain survive better in the infected mice? Protein function is dictated by protein structure, so the authors used computational tools to predict the structure of the protein and the altered protein (with the single-point mutation). They believed the protein could regulate the production of an enzyme called thiol peroxidase. Enzymes are proteins with catalytic activity. In particular, this enzyme played a protective role in the defence against oxidative stress, stress caused by the increased presence of reactive oxygen species (ROS), which are extremely unstable molecules containing oxygen that react with several other molecules within a cell with ease.
So how does it all connect? The infected mice are stressed, and one of the many defence strategies of immune cells in the body is to release reactive oxygen species. Now all the microbes in the gut are at an increased risk of death because of these unstable oxygen-containing molecules reacting with several molecules that are required for the normal functioning of the bacteria. The strains of the bacteria with the single point mutation would have increased protection against reactive oxygen species, so they survive better and dominate the populations. The advantage offered by these strains only holds when they are growing in an environment with high levels of reactive oxygen species. In other words, for uninfected mice, these strains are not special because they do not offer any benefit. Hence, their levels in the populations are a lot lower and even absent. The expansion of the mutant bacteria is a strategy used by B. thetaiotamicron to respond and survive in their modified home (an inflamed gut).
The authors wanted to see whether their observations using the mice model system would hold true in humans. They examined the microbes present in humans of two groups: with inflammatory bowel disease and healthy controls. The authors saw that although the mutated bacteria was present, it was not uniformly present and differed across individuals and over time. The original mouse model was simplistic B. thetaiotamicron was the only microbe apart from the pathogen. In reality, the human gut has many more microbes. While we discussed earlier how the host impacts the microbe and vice-versa, there is a third dimension of interactions. This is the interaction between the microbes themselves. It was found that vitamin B6 was used by the microbes in these interactions. Based on other microbes present, the B. thetaiotamicron population evolved in the infected mice to give rise to the mutated strain. In some cases, the presence of other microbes inhibited the expansion of the mutated strain in the infected mice. This explains the earlier observation with human samples.
This study shows how the microbes in the body respond to cues from the host environment as well as cues from each other. The microbes undergo dynamic changes in response to various cues. These dynamic changes can be used as a signature for the detection of human diseases or can be altered to aid the host organism in fighting off infections.
Featured image: Credit: CC0 Public DomainLink: https://scx1.b-cdn.net/csz/news/800a/2017/gutbacteria.png