Breaking down the microbiology world one bite at a time
No needle, no cry: intranasal SARS-CoV-2 vaccine
The impact of COVID-19
The global COVID-19 pandemic caused by the SARS-CoV-2 virus has had a dramatic impact on human physical and mental health, and the economy. Currently, a full vaccination against SARS-CoV-2 requires several invasive injections and provides immunity for a duration of only 6 months at most. Furthermore, the devastating effects of the pandemic do not affect everyone equally. Factors such as wealth, gender, education and race play a major role in how people across the globe are experiencing the effects of the pandemic .
Despite proven benefits, vaccine hesitancy is still a major global issue. Research scientists are developing new modes of immunisation to overcome some of the problems described above. In order to understand how, it is important to know the basics of how viruses enter our bodies and how vaccinations provide immunity against them.
Viruses, the immune system and vaccines
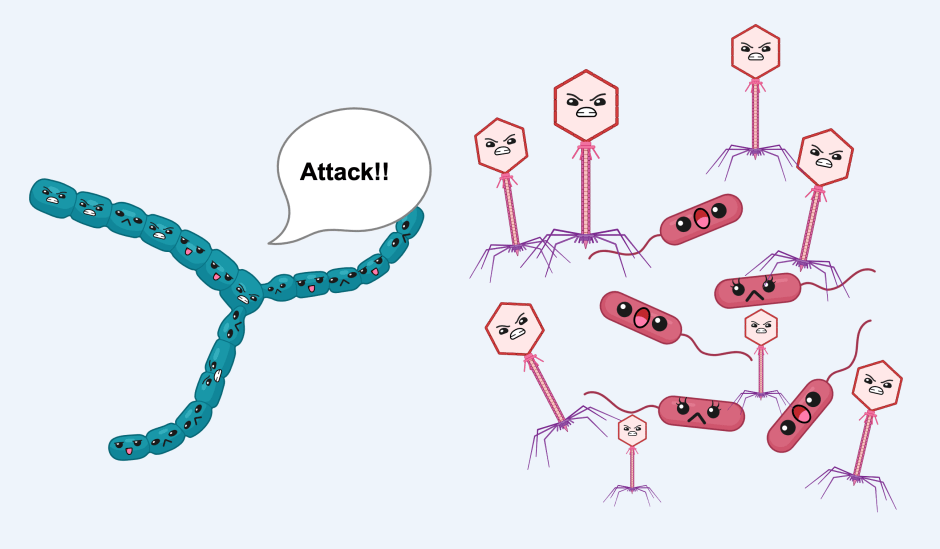
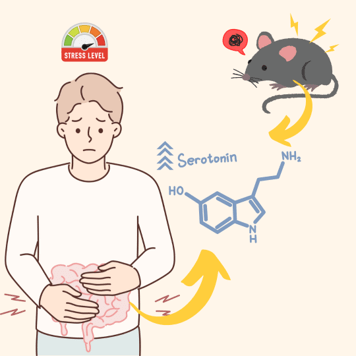
When pathogens, such as viruses, infect us, the innate immune system is our first line of defence (for more information about the innate immune system see here). However, if the virus cannot be dealt with by the innate immune system, the adaptive immune system is activated. The body needs time to activate and deploy the adaptive immune system. However, once it is active, it produces specific antibodies (immunoglobulins) which target and eliminate the viral invader.
Vaccines usually contain an inactive form or just a part of the virus (called an antigen) which simulates a viral infection, but without any real danger. The adaptive immune system is stimulated to produce specific antibodies against the antigen. If the vaccinated person then comes into contact with the real virus, their immune system already has antibodies against that virus and the immune response can quickly eliminate the threat.
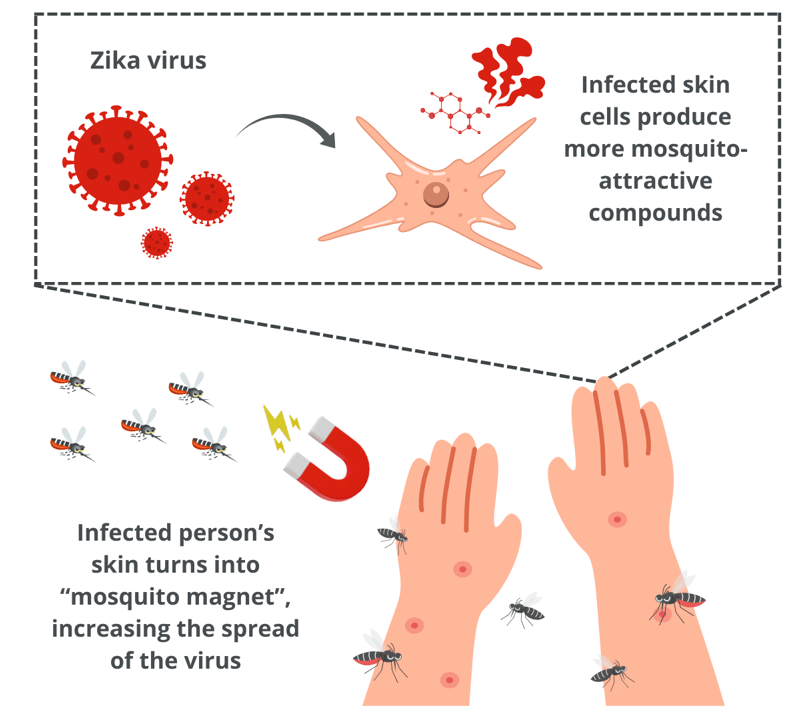
Viruses commonly enter our bodies via our epithelial membranes. Examples include the mucous membranes of the respiratory or the gastrointestinal tract. If the virus is able to pass through the epithelial membrane it can travel into other tissues and circulate around the body via the circulatory system.
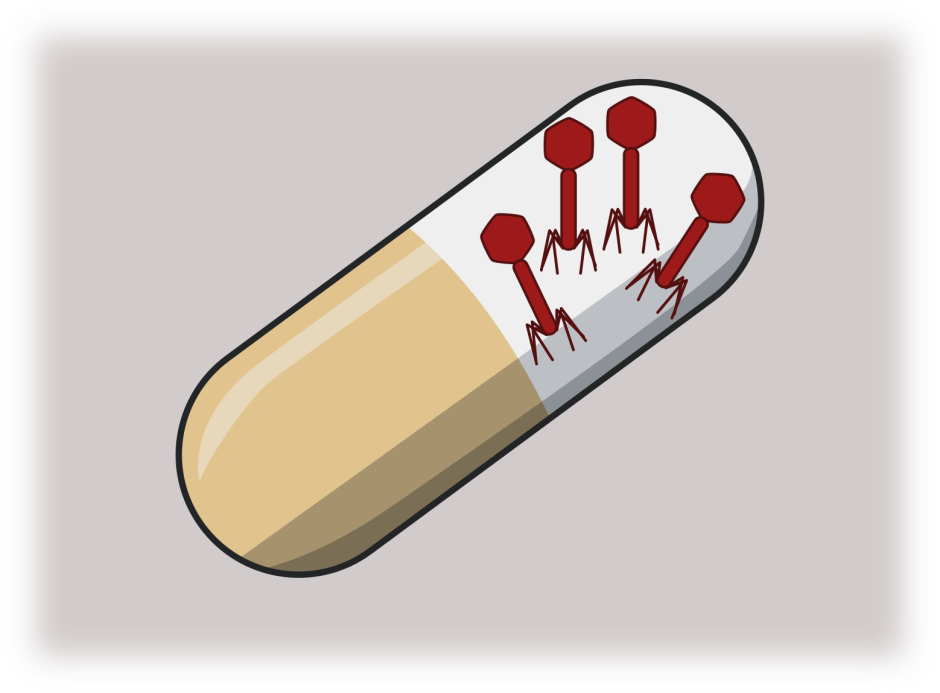
No needle, no cry
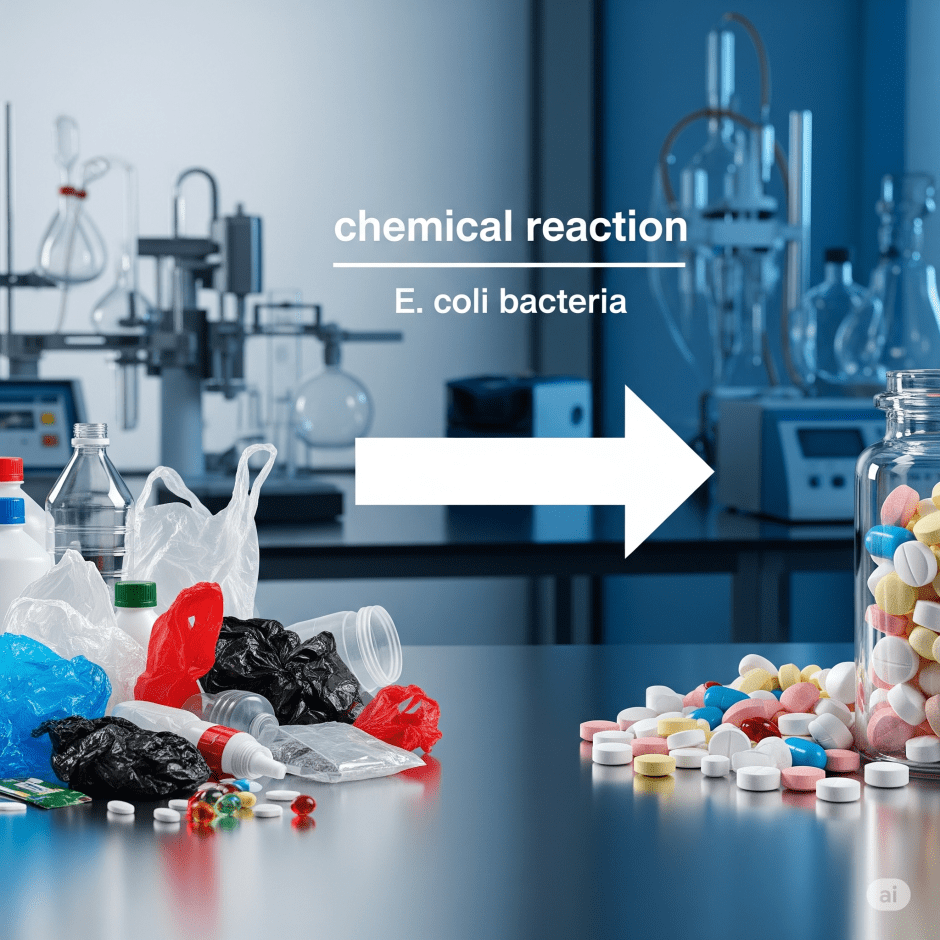
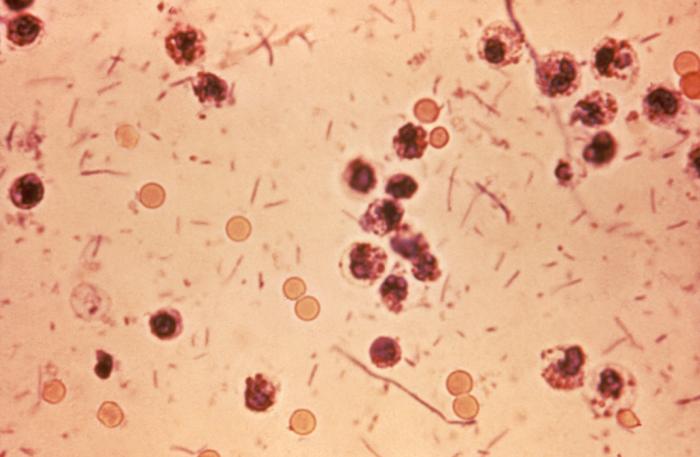
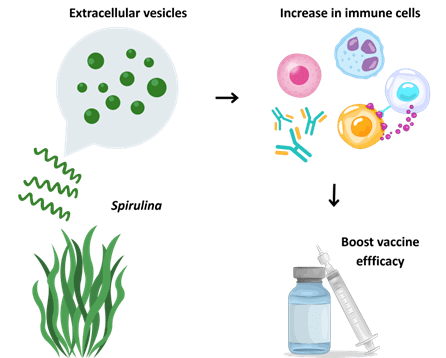
In a current study, the scientists use a highly conserved region of the virus’ spike protein as the antigen. Normally the spike protein allows the virus to stick to and enter through epithelial (outer) membranes. The antigen is delivered to the patient’s body using a strain of L. lactis (Lactococcus lactis) engineered to express the antigen. L. lactis is safe and is already being used to deliver immune therapies due to its status as a generally regarded as safe (GRAS) organism, and its ability to survive the harsh conditions of the human body, needed to deliver the vaccine treatment.
The antigen-expressing L. lactis cells are administered either orally (through the mouth) or nasally (through the nose) to mice. These two methods represent different ways in which viruses most commonly enter the human body. This method is entirely non-invasive and completely bypasses the requirement for invasive needle-based injections.
In the study, three doses of the vaccine are given to the mice over a period of 56 days, at which point the mice are sacrificed for sample collection and analysis. The treatment, and its method of administration, are then analysed to see which results in the most effective immune response. For each condition, a separate group of mice are given L. lactis cells which are not able to express the antigen: this group acts as a negative control (important to note for later).
Intranasal/ oral vaccines stimulate an immune response
The efficiency of the immune response is measured by the changing concentrations of two important immune components:
1. antibodies (immunoglobulins) types IgG and IgA, which are produced and secreted by B-cells and,
2. CD138 expressing B-cells (CD138+) – B-cells are activated in order to produce and secrete antibodies.
IgG is the most common type of antibody, making up a majority of the antibodies in the circulatory system, whereas IgA is predominantly produced by epithelial cells and is found in the mucosal fluid.
56 days after the first vaccination, the researchers find that concentrations of both IgG and IgA significantly increase in response to the treatment, whether its administration was given orally or nasally. This indicates successful stimulation of antibody production in both the circulatory system and in the epithelial membranes regardless of the method of administration.
Interestingly, the CD138+ cell populations of the intestines significantly increase when administered nasally but not orally. Since expression of CD138+ on the surface of B-cells indicates B-cell maturation and antibody production, this implies that nasal administration is more effective.
In addition to measuring the concentrations of IgG, IgA and CD138+ B-cells, the researchers also looked at the populations of CD4+ and CD8+ T-cells in the intestines and lymph nodes, which had significantly increased. This is another important indicator that immunisation promotes effective antibody production.
These results are promising, although the authors note that their negative control showed a low level of IgG/IgA production as well. Despite this, the proof-of-concept study indicates a positive outlook for a new type of vaccine delivery.
The future of intranasal vaccines
The intranasal vaccine shows great promise as an immunotherapy. The vaccine successfully stimulates production of antibodies (the markers of an active adaptive immune response) in a mouse model of infection.
The region of the viral spike protein used in this study is highly conserved, meaning that the vaccine may be effective against other strains of the same virus and possibly other viruses too – although this remains to be tested.
The intranasal vaccine delivery (via a safe L. lactis strain expressing the viral antigen) bypasses the need for invasive injections. Intranasal delivery also provides a faster, more effective barrier, as it occurs directly at the site of viral entry to the body, as indicated by specific stimulation of mucosal IgA.
Future pandemics might be prevented by using a safe, non-invasive nasal spray as was demonstrated in this proof-of-concept study.
Featured image: Original image by author using Adobe Illustrator. .