
Breaking down the microbiology world one bite at a time
Using urine to detect fungal infection
Fungi are becoming an increasingly worrying threat to public health, particularly in individuals who are immunocompromised (those with a weakened immune system). An immune system can become weakened through infection such as human immunodeficiency virus (HIV) and subsequent acquired immunodeficiency syndrome (AIDS), through medication use, an autoimmune condition or cancer, or from organ transplantation. All of these can put an individual at an increased risk of infection, particularly with fungi.
In this study, researchers explored a new diagnostic test for a fungus called Talaromycosis marneffei. This fungus is predominately found in southeast Asia and southern China, however, the range is increasing due to climate change. T. marneffei causes a disease called Talaromycosis mainly in individuals with HIV/AIDS. The mortality (death) rate ranges from 8-40% in this specific patient population with every day of delayed diagnoses increasing the mortality rate by 2% (Zhang et al.). Thus, a quick and accurate diagnostic test is of critical importance as a clinical diagnosis can’t be made due to the nonspecific symptom presentation characteristic of talaromycosis.
The current gold standard diagnostic test is blood culture, but that takes up to 14 days. Tissue can also be biopsied and talaromycosis can be diagnosed using histopathology (microscopic examination of tissue for disease), but this is invasive. A new platform based on antigen (substance that triggers an immune response) detection has been gaining more popularity in China. The antigen used is called Mp1p (mannoprotein) and it is a protein specific to the fungus T. marneffei. This test requires blood sampling, but researchers wanted to know if urine Mp1p could substitute and be just as accurate in diagnosis, particularly in a population of individuals living with AIDS.
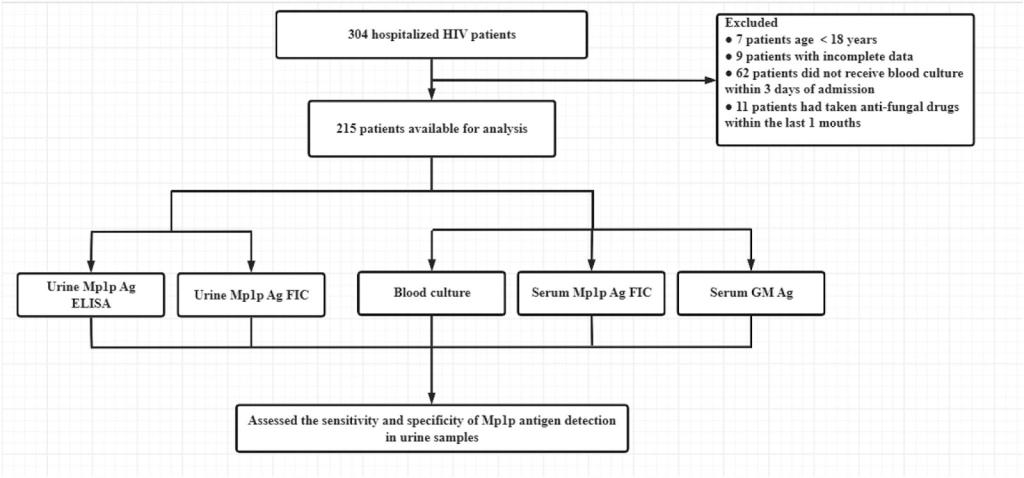
The study consisted of 215 participants, all with HIV+ status. Of the 215, 40 had confirmed T.marneffei infection (blood culture) while 170 were negative. The flow chart of the study design can be seen in Figure 1. Samples from each patient were taken and tested using the 5 conditions outlined in the chart.
What the researchers discovered was that with a urine enzyme linked immunosorbent assay (ELISA) for the Mp1p antigen, the test had a sensitivity of 77.5% and a specificity of 97.1%. Sensitivity is a measure of the ability of a test to correctly identify those with a disease. So in this case, the urine Mp1p ELISA correctly identifies an individual with talaromycosis 77.5% of the time. Specificity is a measure of the ability of a test to correctly identify an individual that doesn’t have disease. Thus, in this case an individual without talaromycosis will return a negative test back 97.1% of the time. The sensitivity of the urine Mp1p antigen test improved significantly when combined with a serum (blood) GM Ag test (test for galactomannan, a component of the fungal cell wall) at 92.5%. An ideal test has high sensitivity and high specificity. For reference, the current blood Mp1p antigen test has a sensitivity in the range of 72-86.3% and a specificity from 96.8-98.1%. A high sensitivity is important to make sure those that have the disease will produce a positive test. A high specificity is important because it will make sure that those who don’t have the disease produce a negative test.
Unfortunately, the blood Mp1p ELISA could not be performed in this study due to limitations, thus it’s difficult to see how the urine Mp1p would match the results if it was performed with a blood culture. Additionally, records weren’t available showing who had already been on antifungal therapy, which could drastically affect results. However, the study did show that Mp1p is secreted in the urine at levels that can be detected. Further research would be needed before this could be a clinically approved diagnostic test, but this paper is a step in the right direction for the development of a less invasive and more accurate detection method for talaromycosis.
Link to the original post: Zhang, Y.; Guo, P.; He, Y.; Zhang, Q.; Yang, L.; Ke, Y.; Meng, Y.; Xu, F.; Tang, X.; Li, L. MP1P antigen detection in urine samples could improve the rapid screening and diagnosis of Talaromycosis marneffei. J. Mycol. Med. 2025, 35, 101553.
Featured image: Fungi in yeast form. | Credit: Deep AI















