Breaking down the microbiology world one bite at a time
The issues of Nontuberculous Mycobacterial Lung Disease
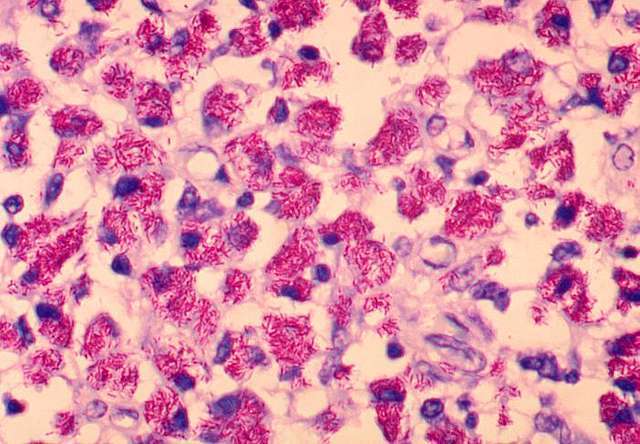
Non-tuberculous mycobacteria (NTM) are a type of bacteria that cause rare infections within the lungs. Those who are the most vulnerable to receiving the infection are patients with damaged lungs or immune system issues.
NTM commonly colonise within the lungs leading to non-tuberculous mycobacteria lung disease (NTM-LD). However, the bacteria can also infect other tissue organs.
In the study, patients with NTM-LD were assessed, and the evidence provided from radiographic and microbiological examinations revealed that NTM were able to surpass and avoid pulmonary macrophages from being engulfed, in the immune defence system. As a result, the bacteria persisted with their colonisation causing the infection to spread. Some of the common symptoms presented by patients with NTM are coughing, phlegm, fatigue and dyspnoea.
Results from experiments such as the meta-analysis showed patients with a large build-up of mucus within the airways, known as bronchiectasis, were the most at risk to contracting NTM-LD. Although bronchiectasis was one of the most important risk factors for NTM-LD, it was the least evaluated risk factor in the study. Nevertheless, patients with abnormal growth of bronchiectasis showed a high correlation with NTM-LD cases.
One of the most known groups of species of NTM is Mycobacterium avium complex (MAC), which contains 12 species, with the most commonly being M. avium, M. intracellulare and M. chimeara. Glycopeptolipids present in the cell wall of MAC assist in the formation of biofilms. This is important for survival of the bacteria against the immune system. One study in 2015 showed MAC accounted for 85% of cases in the US, 83% cases in Europe and 76.2% cases in East Asia; and yet, treatment for NTM-LD has still been difficult due to microbial resistance.
However, the lack of consistent evidence about specifically how the immune system effectively defends itself against NTM in patients has challenged the medical field in finding successful treatment. For example, according to a previous study immune CD4+ T cells were not deficient in patients with NTM pulmonary disease, but were seen reduced in patients during the AIDS pandemic. Also, reports about Interleukin-10 (IL-10), which is an anti-inflammatory cytokine that assists with immune regulation, revealed inconsistent responses in patients with NTM. Results of increased, unchanged or decreased activity of IL-10 in the presence of NTM were witnessed. These show the erratic behavior of the bacteria’s effect in the immune system of the NTM patients.
So, how has treatment for patients with NTM-LD been managed so far?
In 2020, it was reported that successful treatment of NTM-LD required a multidrug administration of 3 to 5 drugs, with a recommended treatment guideline of 18 to 24 months. After 6 months of guideline-based therapy (GBT), patients that continued to show positive sputum cultures of NTM were considered to have refractory (difficult to treat) disease.
However, there are treatments without medicine that patients with NTM-LD can follow and have shown to reduce the condition of the infection. Airway clearance techniques are an example of non-medical treatments for patients. They include procedures such as active cycle of breathing (ACBT), autogenic drainage (AD) and postural drainage.
ACBT focuses on the control of breathing and has shown to reduce symptoms of dyspnoea (difficulty of breathing), asthma and other respiratory symptoms. Postural drainage uses gravity and percussion to loosen the thick mucus,then uses coughing to remove the excess sticky secretion. AD uses various speeds of breathing to remove the mucus and focuses on how fast and deep to breathe to fill certain sections of the lungs with air.
The lack of evidence regarding the treatment and its outcomes for patients with NTM-LD consequently requires further research into how the immune system responds to the disease and how important it is in assisting development of more effective treatment for the future.
Link to the original post: Chien, Y. C., Chang, C. H., Huang, C. K., Chen, Y. H., Liu, C. J., Chen, C. Y., … & Yu, C. J. (2024). The impact of nontuberculous mycobacterial lung disease in critically ill patients: Significance for survival and ventilator use. Journal of Microbiology, Immunology and Infection, 57(2), 328-336. Doi: 10.1016/j.jmii.2023.12.009
Featured image: emoji.sh
Additional sources:
Kim, S., Soon Ho Yoon, Choi, S., Lee, J., Lee, C., Sung Koo Han and Yim, J.-J. (2017). Characteristics associated with progression in patients with nontuberculous mycobacterial lung disease : a prospective cohort study. [online] 17(1). doi:https://doi.org/10.1186/s12890-016-0349-3.
Kumar, K., Aravind Ponnuswamy, Toby GD Capstick, Chen, C., McCabe, D., Hurst, R., Morrison, L., Moore, F., Gallardo, M., Keane, J., Harwood, S., Sinnett, T., Bryant, S., Breen, R., Onn Min Kon, Loebinger, M.R., Lipman, M. and Dhasmana, D.J. (2024). Non-tuberculous mycobacterial pulmonary disease (NTM-PD): Epidemiology, diagnosis and multidisciplinary management. Clinical Medicine, pp.100017–100017. doi:https://doi.org/10.1016/j.clinme.2024.100017.
van Ingen, J., Obradovic, M., Hassan, M., Lesher, B., Hart, E., Chatterjee, A. and Daley, C.L. (2021). Nontuberculous mycobacterial lung disease caused by Mycobacterium avium complex – disease burden, unmet needs, and advances in treatment developments. Expert Review of Respiratory Medicine, [online] 15(11), pp.1387–1401. doi: https://doi.org/10.1080/17476348.2021.1987891.
http://www.cff.org. (2024). Autogenic Drainage (AD) | Cystic Fibrosis Foundation. [online] Available at: https://www.cff.org/managing-cf/autogenic-drainage-ad